The Covid response at the VA Illiana Health Care System facility in Danville was mismanaged according to the Veteran Affairs Office of the Inspector report released Oct. 21. | Flickr
The Covid response at the VA Illiana Health Care System facility in Danville was mismanaged according to the Veteran Affairs Office of the Inspector report released Oct. 21. | Flickr
The Covid response at the VA Illiana Health Care System facility in Danville was mismanaged according to the Veteran Affairs Office of the Inspector report released Oct. 21.
The Covid infection killed 11 veterans. The report said leaders at the nursing home did not follow appropriate Covid guidelines during the outbreak and that staff were warned about pouting elderly veterans in danger.
Read the full report below:
Office of Healthcare Inspections
VETERANS HEALTH ADMINISTRATION Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at VA Illiana Health Care System in Danville, Illinois
HEALTHCARE INSPECTION REPORT #21-00553-285 SEPTEMBER 28, 2021

In addition to general privacy laws that govern release of medical
information, disclosure of certain veteran health or other private
information may be prohibited by various federal statutes including, but
not limited to, 38 U.S.C. §§ 5701, 5705, and 7332, absent an exemption or other specified circumstances. As mandated by law, the OIG adheres to
privacy and confidentiality laws and regulations protecting veteran health or other private information in this report.
Report suspected wrongdoing in VA programs and operations to the VA OIG Hotline:
www.va.gov/oig/hotline
1-800-488-8244
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a
``
Community Living Center at the VA Illiana HCS in Danville, IL
Executive Summary
The VA Office of Inspector General (OIG) conducted a healthcare inspection to assess allegations that facility leaders failed to mitigate risk of and manage a community living center (CLC) COVID-19 outbreak (CLC outbreak) at the VA Illiana Health Care System (facility) in Danville, Illinois.1In the fall of 2020, 11 residents died of COVID-19, and 239 patients and 92 staff were diagnosed with the virus. The allegations stated that a COVID-19 outbreak occurred in two CLC neighborhoods—Unity and Victory—and there was a failure to observe general infection control practices specifically related to respiratory personal protective equipment (PPE) use, issuance, and training; failure to minimize risk of exposure to COVID-19 for CLC residents and staff; and inconsistent ongoing testing and failure to notify residents, their families, and staff of positive COVID-19 test results. The OIG identified concerns related to facility and CLC leaders’ actions following the CLC outbreak.2
Infection control measures limit the spread of transmissible diseases and include wearing basic PPE, such as face masks, and more specialized items such as respirators. The OIG substantiated that facility leaders and staff failed to observe general infection control practices specifically related to respiratory PPE including face coverings, face masks, N95s, and powered air purifying respirators (PAPRs).
Facility and CLC leaders took steps to emphasize and reinforce the importance of staff wearing face masks properly. The Facility Director stated support of facility supervisors taking disciplinary action for staff who were noncompliant. However, the OIG found that CLC residents did not consistently wear face coverings prior to the CLC outbreak and a few CLC staff did not comply with infection control measures related to face masks both prior to, and after, the
1 The underlined terms are hyperlinks to a glossary. To return from the glossary, press and hold the “alt” and “left arrow” keys together.
2 On March 11, 2020, due to the “alarming levels of spread and severity” of COVID-19, the World Health Organization declared a pandemic. For the purposes of this review, the OIG defined the duration of the CLC outbreak to be from the date the first CLC employee tested positive through the date of death of the last resident diagnosed with COVID-19 (October 13–November 17, 2020).
VA OIG 21-00553-285 | Page i | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
CLC outbreak.3 Moreover, the OIG did not identify any disciplinary actions brought against staff for noncompliance with infection control practices.
The OIG substantiated that at the time of the CLC outbreak, the facility’s Environmental and Safety Section did not identify CLC providers and nursing staff as requiring respiratory protection.4 The facility’s Safety Manager justified this decision by noting that prior to the CLC outbreak, there was a lack of contagious diseases in the CLC units. Although not identified by the facility’s Environmental and Safety Section, the OIG found some CLC providers and one CLC nursing staff member on the impacted units were N95 mask fit tested prior to the CLC outbreak. According to facility records, none of the nursing staff on Unity and Victory had PAPR training prior to the outbreak. This failure resulted in CLC nursing staff providing direct care to residents with suspected and confirmed diagnoses of COVID-19 without the preferred respiratory protection.5
The OIG substantiated that CLC and facility leaders failed to minimize the risk of CLC residents and staff exposure to COVID-19. Facility leaders did not follow Centers for Disease Control and Prevention (CDC) guidance when responding to a CLC staff member’s reported cough and COVID-19 community close contact exposure, and did not remove the employee from direct patient care. Information as to why this occurred was conflicting. A few interviewees stated that the notification went through the chain of command and ultimately the Acting Associate Director of Patient Care Services was contacted and gave instructions that the CLC staff member would not be tested and should wear a mask and remain at work. However, the Acting Associate Director of Patient Care Services reported having no knowledge of this event. The Chief of Geriatrics and Rehabilitation Service arranged for the staff member to be tested the day after reporting the close contact exposure. The test result was positive for COVID-19. The failure to
3“Interim Infection Prevention and Control Recommendations for Healthcare Personnel During the Coronavirus Disease 2019 (COVID-19) Pandemic,” Centers for Disease Control and Prevention (CDC), accessed on January 21, 2021, https://stacks.cdc.gov/view/cdc/90582. Face coverings are most often cloth and are not considered PPE. “Personal Protective Equipment: Questions and Answers,” CDC, accessed on June 7, 2021. http://web.archive.org/web/20201001160417/https://www.cdc.gov/coronavirus/2019-ncov/hcp/respirator-use faq.html. Face masks refer to non-FDA regulated procedure masks as well as surgical masks and provide barrier protection against droplets, including large respiratory particles, and are intended to prevent contamination of the surrounding area when the wearer coughs or sneezes. Face masks do not require fit testing. Proper wearing of face masks is demonstrated when each loop is around the ears, the bendable edge of the mask is around the bridge of the nose, the mask covers the nose and mouth, and the lower edge of the mask is under the chin. 4 For this report, the OIG considers providers to include physicians, nurse practitioners, and physician assistants. Facility MCM 001ESS-11, Respiratory Protection Program, December 2017. The facility’s Respiratory Protection Program is specific to respiratory protection provided by N95s and PAPRs.
5“Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) in Healthcare Settings,” CDC, accessed on April 22, 2021. https://stacks.cdc.gov/view/cdc/86043. Preferred respiratory protection for CLC staff providing care to COVID-19 infected residents include fit tested N95s or PAPRs.
VA OIG 21-00553-285 | Page ii | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
remove the staff member, who tested positive for COVID-19, resulted in the employee providing direct patient care and potentially exposing CLC residents and staff to COVID-19.
Veterans Health Administration (VHA) guidance for CLCs dated March 17, 2020, stated, “the facility should have a plan to isolate a resident that is suspected of having COVID-19.” VHA guidance defers to each facility to determine the specifics related to managing the transfer and isolation of residents suspected of having, or diagnosed with, COVID-19.6 The OIG found the
facility did not have a comprehensive plan that specified operational details such as roles, actions, and targeted time frames for transfer and isolation of CLC residents suspected of, or diagnosed with, COVID-19. The lack of a plan was likely a contributory factor for two COVID 19 positive residents remaining at the CLC for 20 hours after a CLC physician was notified of the positive diagnoses. One of the residents diagnosed with COVID-19 stayed overnight in a room with a roommate who was COVID-19 negative. Once the resident was transferred, the shared room was cleaned. However, due to an inoperable bed management system and the lack of an alternative system of record keeping, the OIG was unable to determine when the cleaning occurred.
The OIG determined that due to a lack of knowledge of infection control requirements, facility and CLC leaders did not implement additional measures recommended by the CDC when administering aerosol-generating procedures such as nebulizers, that produce spray and droplets and run the risk of introducing the virus into the air. The failure of CLC leaders to disseminate this information resulted in two residents receiving aerosol-generating procedures without the proper infection control measures in place.
In response to the risks associated with transmission of COVID-19, VHA guidance stated that facilities with CLCs should immediately initiate procedures to cancel all group activities.7 The OIG team found CLC leaders permitted group therapy sessions to continue throughout the pandemic and that facility leaders were unaware that group therapy sessions were taking place. The OIG identified that two Unity residents tested positive for COVID-19 the same day after they attended separate group therapy sessions with five other residents. Similarly, three of the first four Victory residents diagnosed with COVID-19 attended a group therapy session three days earlier with six other residents. Continuation of group therapy sessions during the pandemic increased the risk of exposure to COVID-19 for CLC residents and staff.
Concerns regarding the separation of nurses working with residents diagnosed with COVID-19 from residents without the diagnosis during the same shift led the OIG team to review nurse staffing assignments. The OIG found that CLC leaders minimized the risk of cross
6 VHA Memorandum, Coronavirus (COVID-19) Community Living Centers – Revised 03/17/2020. 7 VHA Memorandum, Coronavirus (COVID-19) Community Living Centers – Revised 03/17/2020.
VA OIG 21-00553-285 | Page iii | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
contamination by ensuring staff did not work on both the COVID-19 and non-COVID-19 designated units during the same shift.
Testing for COVID-19 provides facility staff with information regarding disease activity among CLC residents and staff.8 The OIG found the facility lacked a plan for post-baseline testing of residents and staff and that ongoing testing following the CLC outbreak was inconsistent. The absence of a post-baseline plan resulted in the lack of a standardized process to address ongoing disease screening, monitoring, and testing of CLC residents and staff for the prevalence of COVID-19. In addition, the OIG learned that there was no formalized process for tracking weekly COVID-19 testing of residents and staff. The failure to test represents a missed opportunity to promptly identify and isolate residents and staff diagnosed with COVID-19 to reduce further transmission of the virus and may have led to staff members working while having COVID-19. The OIG did not substantiate that the facility failed to notify residents, their families, and staff about COVID-19 test results.
The OIG team identified a failure by facility leaders to proactively develop and implement plans to prepare for, and respond to, a potential COVID-19 outbreak at the CLC following VHA’s identification of CLCs as a high-risk environment.9 The OIG found the facility’s initial action plan, prepared prior to the official recognition of the pandemic, lacked planning specific to CLC preparedness for mitigating or responding to COVID-19. Rather, facility leaders focused on planning for an influx of VHA patients from other geographic regions or non-VHA patients from the community who may have needed to be quarantined at the facility due to a lack of beds elsewhere. Facility leaders did not initiate CLC-specific planning until the CLC outbreak occurred, seven months into the pandemic. Analysis by the OIG team identified the lack of CLC specific planning as a contributory factor that led to a failure to identify CLC staff as: requiring respiratory protection, being fit tested and issued N95 masks, and trained in the use of PAPRs; developing thorough processes to minimize exposure; and ensuring consistent testing for residents and staff. The failure to proactively develop and implement plans was a missed opportunity to ensure that facility and CLC staff were in a state of ongoing readiness should a CLC resident or staff member become diagnosed with COVID-19.
Facility leaders developed a post-COVID-19 outbreak action plan following the CLC outbreak. This plan was based on concerns identified by administrative nurses who provided direct patient care during the CLC outbreak and led to six teams focusing on the concerns. While the input of
the administrative nurses was considered, CLC direct care staffs’ input was not included. The OIG determined that, while the plan was a step in the right direction, actions taken by facility and CLC leaders following the CLC outbreak lacked input of frontline staff to identify corrective
8 VHA Memorandum, COVID-19 Guidance on COVID-19 Testing for Community Living Centers and Spinal Cord, June 11, 2020.
9 VA Response to COVID-19, Guidance for VA Community Living Centers, March 6, 2020.
VA OIG 21-00553-285 | Page iv | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
actions and opportunities for improvement. A review of vaccination data showed the facility had made significant progress toward mitigation of the spread of COVID-19 through vaccines; all CLC residents were fully vaccinated as of March 9, 2021.
The OIG made one recommendation to the Veterans Integrated Service Network Director related to administrative actions and 14 recommendations to the Facility Director related to face mask compliance, staff training on and access to respiratory PPE, limiting exposure to COVID-19 for residents and staff, tracking the completion of room cleaning, following CDC guidelines for aerosol-generating procedures, disseminating new or updated VHA policies, maintaining oversight of CLC implementation of VHA guidance, completing a post-baseline testing plan, reviewing facility procedures for the timely management of individuals with positive COVID-19 test results, performing ongoing testing of residents and staff, notifying family members of a resident’s change in condition, identifying and planning for high-risk scenarios, and including frontline staff in after-action reviews of the CLC outbreak.
Comments
The Veterans Integrated Service Network and Facility Directors concurred with the findings and recommendations 1–14 and concurred in principle with recommendation 15. Acceptable action plans were provided (see appendixes D and E for the Directors’ comments). The OIG considers all recommendations open and will follow up on the planned actions until they are completed.
JOHN D. DAIGH, JR., M.D.
Assistant Inspector General
for Healthcare Inspections
VA OIG 21-00553-285 | Page v | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
Contents
Executive Summary......................................................................................................................... i Abbreviations............................................................................................................................... viii Introduction......................................................................................................................................1 Scope and Methodology ..................................................................................................................3 Timeline of Events...........................................................................................................................4 Inspection Results............................................................................................................................9
Allegation: Failure to Observe General Infection Control Practices Specific to Respiratory PPE......................................................................................................................9
Allegation: Failure to Minimize Risk of Exposure to COVID-19............................................13
Allegation: Inconsistent Ongoing Testing and Failure to Notify of Positive COVID-19 Test Results...............................................................................................................22
Contributory Factors .................................................................................................................27 Concern: Facility and CLC Leaders’ Post-CLC Outbreak Actions..........................................29 Conclusion .....................................................................................................................................31 Recommendations 1–15.................................................................................................................33 Appendix A: Facility Campus Map ...............................................................................................35 Appendix B: Facility Inpatient Surge Plan ....................................................................................36 Appendix C: CLC Upsurge Action Plan........................................................................................37 Appendix D: VISN Director Memorandum ..................................................................................39
VA OIG 21-00553-285 | Page vi | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
Appendix E: Facility Director Memorandum................................................................................41 Glossary .........................................................................................................................................49 OIG Contact and Staff Acknowledgments ....................................................................................53 Report Distribution ........................................................................................................................54
VA OIG 21-00553-285 | Page vii | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
Abbreviations
ADPCS Associate Director of Patient Care Services CDC Centers for Disease Control and Prevention CLC Community Living Center
CPAP continuous positive airway pressure EHR electronic health record
NOD Nurse Officer on Duty
OIG Office of Inspector General
PAPR powered air purifying respirator PPE personal protective equipment SOP standard operating procedure VHA Veterans Health Administration VISN Veterans Integrated Service Network
VA OIG 21-00553-285 | Page viii | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a
``
Community Living Center at the VA Illiana HCS in Danville, IL
Introduction
The VA Office of Inspector General (OIG) conducted a healthcare inspection to assess allegations that facility leaders failed to mitigate risk of and manage a community living center (CLC) COVID-19 outbreak (CLC outbreak) at the VA Illiana Health Care System (facility) in Danville, Illinois.1
Background
The facility, part of Veterans Integrated Service Network (VISN) 12, consists of an acute care medical center, primary care and mental health clinics, and a CLC. The facility is designated as Level 3, low complexity, and has 38 inpatient beds for internal medicine and psychiatry, and a 109 bed CLC.2 The facility does not have an intensive care unit or an emergency department. The main CLC, located in Building 101, is divided into four neighborhoods and provides services in “rehabilitation, dementia and Alzheimers care, geri-psychiatric care, palliative care and extended care.”3 Additionally, the CLC includes four smaller, free-standing homes on the facility campus called Green Houses, which provide the same services found at the main CLC (see appendix A).4
COVID-19 Impact on Residents of Nursing Homes and CLCs
As of February 25, 2021, nursing home resident deaths accounted for 35 percent of all United States deaths due to COVID-19, even though fewer than 1 percent of the population reside in nursing homes.5 This highlights the risk of death from COVID-19 in residents who are older, may have complex medical conditions, and may be immunocompromised.6“Older adults and people who have severe underlying medical conditions like heart disease or lung disease or
1 Underlined terms are hyperlinks to a glossary. To return from the glossary, press and hold the “alt” and “left arrow” keys together.
2 VHA Office of Productivity, Efficiency, and Staffing, The Facility Complexity Model classifies VHA facilities at levels 1a, 1b,1c, 2, or 3, with level 1a being the most complex and level 3 being the least complex. A level 3 facility has low volume, low risk patients; few, or no complex clinical programs; and small or no research and teaching programs.
3“VA Illiana Health Care System,” VA Intranet, Facilities Locator and Leadership Directory, accessed November 13, 2020. The four neighborhoods are known as Unity, Victory, Abe Lincoln Boulevard, and Stars and Stripes. Two other units that were vacant pre-pandemic were also located in Building 101. The two vacant units were not designated as neighborhoods with specific names and were known as 101-1 and 101-2.
4 The four Green Houses are known as Freedom, Honor, Liberty, and Valor.
5 VHA Handbook 1142.01, Criteria and Standards for VA Community Living Centers (CLC), August 13, 2008. The handbook announced VA’s decision to replace the term nursing home care unit with community living center. For the purpose of this review, the OIG refers to CLC patients as residents.
6 Orestis A. Panagiotou et al., “Risk Factors Associated With All-Cause 30-Day Mortality in Nursing Home Residents With COVID-19,” JAMA Internal Medicine, (January 4, 2021): 2.
VA OIG 21-00553-285 | Page 1 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
diabetes seem to be at higher risk for developing more serious complications from COVID-19 illness.”7 Additionally, nursing home residents live in close proximity to one another requiring significant hands-on care from staff, thus increasing transmission risks for certain infections including COVID-19. Further, residents with cognitive or mental disorders may be noncompliant with wearing personal protective equipment (PPE) and may wander, promoting the spread of COVID-19 and limiting mitigation efforts in an outbreak. A recent study of nursing home residents also recognized increased age, masculine gender, and impaired cognitive and physical function as risk factors for COVID-19 mortality.8 These demographics in mortality risks are comparable to those residents who live in VA CLCs.9
Prior OIG Reports
In March 2020, the OIG conducted an inspection to evaluate Veterans Health Administration’s (VHA) COVID-19 screening processes and pandemic readiness at selected VA medical facilities. The OIG observed staff conducting screenings at acute care facilities and CLCs, and interviewed VHA leaders on their facilities’ readiness capabilities.10 The facility at issue in this report was included in the review and the OIG found (1) the facility reported adequate supplies and equipment, and (2) access to the CLC was limited, per VHA policy.11
Allegations and Concerns
On October 21 and 22, 2020, the OIG received two separate complaints alleging that facility leaders failed to mitigate risk of and manage a COVID-19 outbreak at two CLC neighborhoods, Unity and Victory. Due to the nature of the allegations and the impact of COVID-19 on the vulnerable CLC population, the OIG opened a hotline inspection on November 6, 2020, to review the care of the residents, implementation of and adherence to VHA guidance for CLCs related to COVID-19, and facility leaders’ management of the CLC outbreak.
7“Symptoms of Coronavirus,” Center for Disease Control and Prevention, accessed on November 19, 2020. https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html.
8 Panagiotou, “Risk Factors,”
9 VA OIG, Review of VHA Community Living Centers and Corresponding Star Ratings, Report No. 18-05113-81, February 12, 2020. VHA Handbook 1142.01.
10 VA OIG, OIG Inspection of Veterans Health Administration COVID-19 Screening and Pandemic Readiness, Report No. 20-02221-120, March 26, 2020.
11 VA OIG, Report No. 20-02221-120, March 26, 2020. “VA announces safeguards to protect nursing home and spinal cord injury patients,” Office of Public and Intergovernmental Affairs, accessed February 9, 2021 https://www.va.gov/opa/pressrel/pressrelease.cfm?id=5400. On March 10, 2020, VA instituted a “no visitors stance” at CLCs and spinal cord injury units.
VA OIG 21-00553-285 | Page 2 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
The complainants alleged
∙ failure to observe general infection control practices specifically related to respiratory PPE use, issuance, and training,
∙ failure to minimize risk of exposure to COVID-19 for CLC residents and staff, and
∙ inconsistent ongoing testing and failure to notify residents, their families, and staff of positive COVID-19 test results.
During the inspection, the OIG identified concerns related to facility and CLC leaders’ post outbreak actions. Additionally, the OIG learned of a concern that facility leaders failed to address the emotional well-being of CLC staff after the CLC outbreak. This was discussed with OIG leaders and is under review through other ongoing OIG work. As such, it is not addressed in this report.
Scope and Methodology
The OIG initiated the inspection on November 6, 2020, and conducted a virtual site visit December 14–17, 2020. Additionally, an unannounced site visit was completed on February 17, 2021. The OIG defined the duration of the CLC outbreak to be from the date the first CLC employee tested positive through the date of death of the last resident diagnosed with COVID-19 (October 13–November 17, 2020).
The OIG interviewed staff familiar with the CLC outbreak and actions taken following the outbreak. Interviewees included the Facility Director, Acting Chief of Staff, Acting Associate Director of Patient Care Services (ADPCS), Chief of Geriatrics and Rehabilitation Service, Acting Chief Nurse of Geriatrics, and CLC nursing staff.
The OIG team reviewed the electronic health records (EHR) of CLC residents, employee health records of staff, VHA and facility policies, VHA operational memorandums, facility standard operating procedures (SOPs) and statements of work, Centers for Disease Control and Prevention (CDC) COVID-19 guidance, Geriatric and Rehabilitation Service meeting minutes, facility town hall COVID-19 meeting minutes, Employee Health testing data, N95 fit testing and powered air-purifying respirator (PAPR) training records, nursing staff schedules, and facility COVID-19 action plans from March 2020 through February 2021.
In the absence of current VA or VHA policy, the OIG considered previous guidance to be in effect until superseded by an updated or recertified directive, handbook, or other policy document on the same or similar issue(s).
The OIG substantiates an allegation when the available evidence indicates that the alleged event or action more likely than not took place. The OIG does not substantiate an allegation when the available evidence indicates that the alleged event or action more likely than not did not take
VA OIG 21-00553-285 | Page 3 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
place. The OIG is unable to determine whether an alleged event or action took place when there is insufficient evidence.
Oversight authority to review the programs and operations of VA medical facilities is authorized by the Inspector General Act of 1978, Pub. L. No. 95-452, 92 Stat. 1101, as amended (codified at 5 U.S.C. App. 3). The OIG reviews available evidence to determine whether reported concerns or allegations are valid within a specified scope and methodology of a healthcare inspection and, if so, to make recommendations to VA leaders on patient care issues. Findings and recommendations do not define a standard of care or establish legal liability.
The OIG conducted the inspection in accordance with Quality Standards for Inspection and Evaluation published by the Council of the Inspectors General on Integrity and Efficiency.
Timeline of Events
Prevalence of COVID-19
On March 11, 2020, due to the “alarming levels of spread and severity” of COVID-19, the World Health Organization declared a pandemic.12
Danville, Illinois, has a population of 30,000 people and is located in Vermilion County, roughly 1.5 hours west of Indianapolis, Indiana, and 2.5 hours south of Chicago, Illinois. Figure 1 depicts the number of persons diagnosed with COVID-19 for Vermilion County from March 15 through November 30, 2020.13
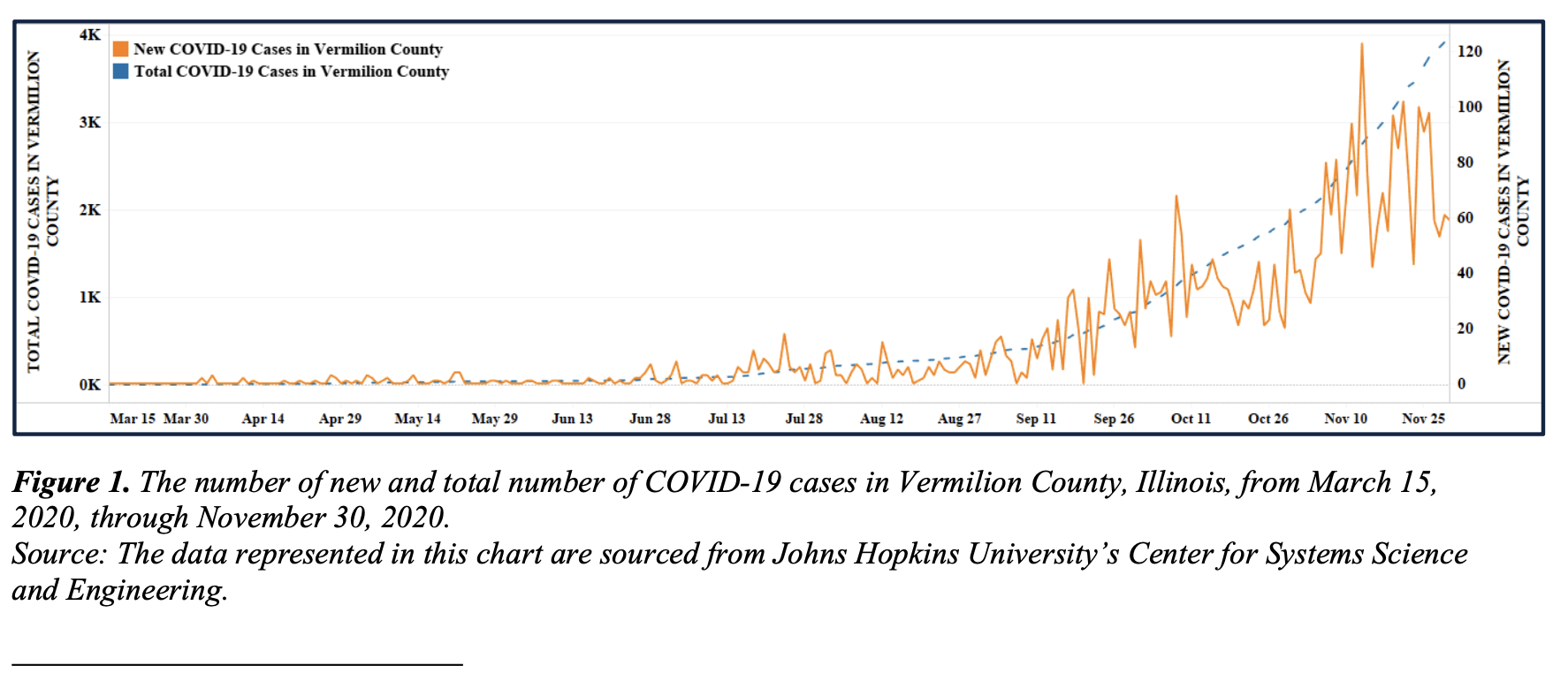
Figure 1. The number of new and total number of COVID-19 cases in Vermilion County, Illinois, from March 15, 2020, through November 30, 2020.
Source: The data represented in this chart are sourced from Johns Hopkins University’s Center for Systems Science and Engineering.
12 World Health Organization, WHO Director-General’s opening remarks at the media briefing on COVID-19, March 11, 2020, accessed on November 19, 2020, https://www.who.int/dg/speeches/detail/who-director-general-s opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020.
13“COVID-19 United States Cases by County,” Johns Hopkins University, accessed March 9, 2021, https://github.com/CSSEGISandData/COVID-19.
VA OIG 21-00553-285 | Page 4 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
The facility employs roughly 1500 people. Figure 2 depicts the number of facility staff diagnosed with COVID-19 from March 15, 2020, through November 30, 2020.14 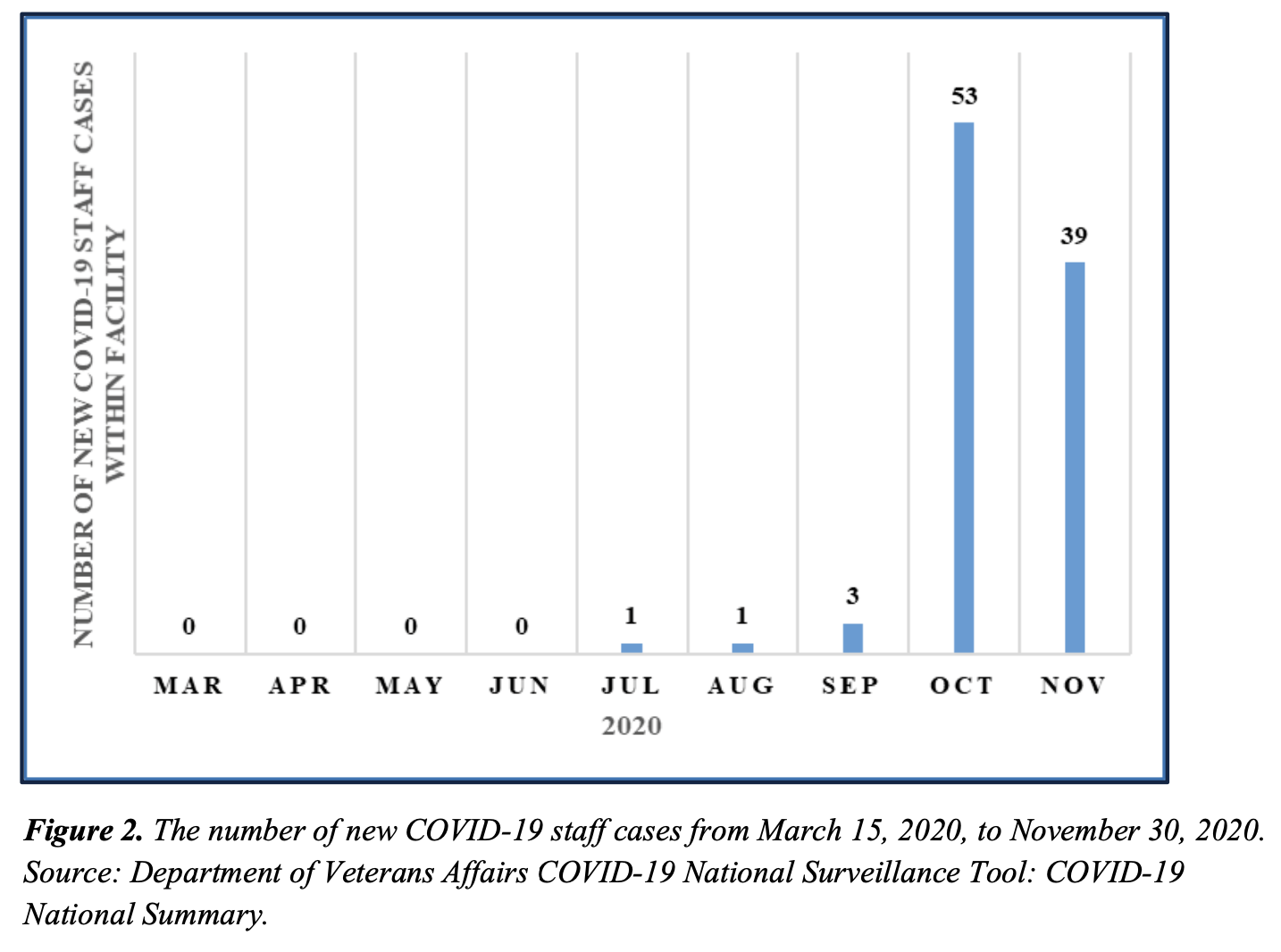
Figure 2. The number of new COVID-19 staff cases from March 15, 2020, to November 30, 2020. Source: Department of Veterans Affairs COVID-19 National Surveillance Tool: COVID-19 National Summary.
The facility served over 29,000 veterans from October 1, 2019, through September 30, 2020. Figure 3 depicts the number of veterans, both inpatient and outpatient, newly diagnosed with COVID-19 at the facility from March 15, 2020, through November 30, 2020.15
14 VA National Surveillance Data, accessed March 8, 2021.
15 VA National Surveillance Data, accessed March 8, 2021.
VA OIG 21-00553-285 | Page 5 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a
Community Living Center at the VA Illiana Health Care System in Danville, IL
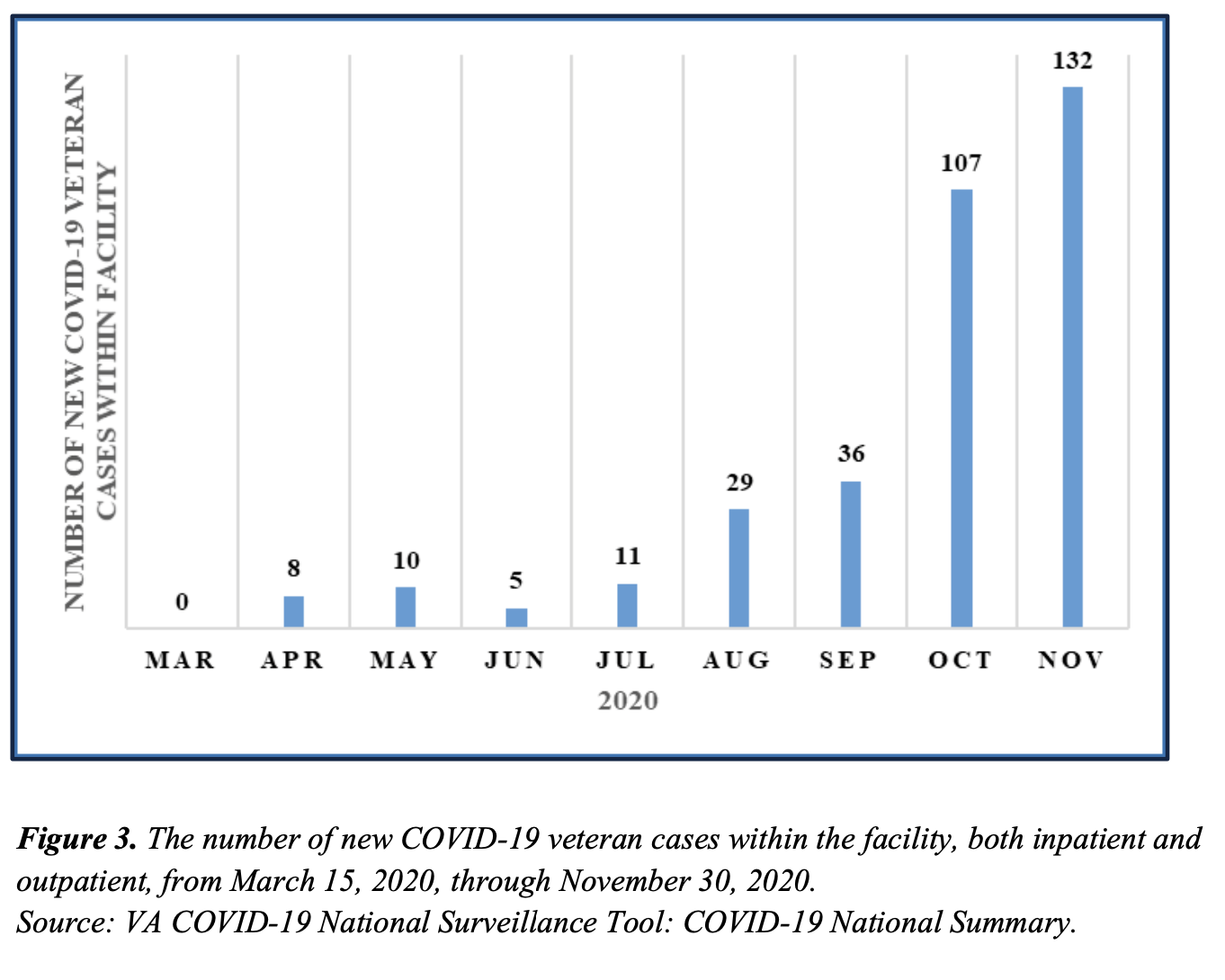
Figure 3. The number of new COVID-19 veteran cases within the facility, both inpatient and outpatient, from March 15, 2020, through November 30, 2020.
Source: VA COVID-19 National Surveillance Tool: COVID-19 National Summary.
COVID-19-Related Facility Actions and Occurrences
Consistent with VHA guidance, the facility developed a pandemic action plan in January 2020, that included 46 items addressing topics such as screening processes for staff and visitors, COVID-19 staff education, signage, documentation templates, and PPE inventory. Target dates for completion of the items ranged from January 27 to March 21, 2020. The action plan assessed the need for respiratory PPE for staff working in some facility locations and services. However, it did not include actions to minimize or address a potential outbreak at the facility’s CLC.16
The Facility Director held daily virtual town hall meetings to communicate COVID-19-related updates to staff from March 12–31, 2020, after which the frequency was reduced to three times per week. Additionally, the facility had a COVID-19 information SharePoint site available for
staff reference. The facility linked its website to VHA’s COVID-19 SharePoint site available for staff.
A facility pandemic incident command center (command center) opened on March 23, 2020, to manage COVID-19 related information and decisions. The command center had a dedicated phone line and email address that staff could use to ask COVID-19 associated questions. At the same time, facility leaders started planning for an influx of patients from the community.
16 The information provided in this section is based on a review of documents and interviews with the facility Director, Acting ADPCS, Chief of Facilities Management, and the infection control coordinator.
VA OIG 21-00553-285 | Page 6 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
As noted in figures 1, 2, and 3, the county and facility experienced a low number of newly diagnosed COVID-19 cases through the spring and summer of calendar year 2020.
Low rates of COVID-19 at the county level resulted in the facility experiencing minimal impact from the pandemic in the initial months. Therefore, the Facility Director reduced the frequency of the virtual town halls to once a week on May 18, 2020; the command center was “stood down” on June 25, 2020.17 With the command center no longer staffed, command center members met virtually as needed and the email and phone number remain active for staff to use for COVID-19-related concerns.
In July 2020, the number of individuals testing positive for COVID-19 started to increase in the community. The Valor House, a Green House with a maximum capacity of 10 residents, was closed due to low census and repurposed as a potential quarantine space. Table 1 is a timeline of events that occurred in the facility and CLC planning, decision-making, and outcomes specific to COVID-19.
Table 1. Timeline of Notable Events Related to the CLC COVID-19 Outbreak
| Location |
| Freedom House |
| Valor House |
| Freedom House |
| Victory |
| Victory |
| Unity |
| Victory |
| Victory |
| Unity |
Date Event
August 2020 Residents transferred to Valor House from Freedom House
because of the need for repairs.
August 29–September 5, 2020 Two staff and three residents tested positive for COVID-19.
End of September 2020 All residents who had temporarily relocated to Valor
House returned to Freedom
House.
October 13, 2020 One staff member tested positive for COVID-19.
October 13, 2020 All residents tested negative for COVID-19.
October 14, 2020 All residents tested negative for COVID-19.
October 17, 2020 One staff member tested positive for COVID-19.
October 18, 2020 Two staff and four residents tested positive for COVID-19.
October 19, 2020 Four staff tested positive for COVID-19.
17 Merriam-Webster, “Definition of Stand down, or when used as a verb, stood down,” accessed April 16, 2021, https://www.merriam-webster.com/dictionary/stand-down. A term that indicates going off duty or ending operations.
VA OIG 21-00553-285 | Page 7 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
| Location |
| Liberty House |
| Valor House |
| Unity |
| 101-2 |
| 101-2 |
| Facility |
| Facility |
| Facility |
| Unity and Victory |
| 101-1 |
Date Event
October 19, 2020 One resident tested positive for COVID-19.
October 19, 2020 Five COVID-19 positive residents from Victory and
Liberty House transferred to
Valor House.
October 20, 2020 All residents retested; two tested positive for COVID-19.
October 21, 2020 Facility leaders opened 101-2 for COVID-positive residents
due to limited capacity in the
Valor House.
October 21, 2020 CLC staff transferred nine COVID-19 positive residents to
101-2; two from Unity, two from
Victory, and five from Valor
House.
October 22, 2020 Facility leaders finalized inpatient surge plan (see
Appendix B).
October 22, 2020 CLC leaders finalized CLC Upsurge Plan (see Appendix C).
October 23, 2020 Facility leaders opened a second unused unit, 101-1, and
approved moving all COVID-19
negative CLC residents from
Unity and Victory to allow
cleaning of the space.
October 23, 2020 All remaining residents retested; two from Unity and two from
Victory tested positive for
COVID-19 and were transferred
to 101-2.
October 24, 2020 CLC staff transfer the12 remaining residents on Unity
and Victory to 101-1.
Source: OIG analysis of timeline using EHRs and facility documents.
In October, following the CLC outbreak, command center meetings resumed with a frequency of once a week. From the date the first resident tested positive for COVID-19 at the CLC, to the date of the last death of a resident diagnosed with COVID-19, approximately one month, 11 residents died after having tested positive for COVID-19. Seven of the 11 residents had documentation in their EHR stating their death was from COVID-19-related respiratory complications, and four of the 11 residents had other causes noted as the primary cause of death but accelerated by COVID-19.
VA OIG 21-00553-285 | Page 8 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
Inspection Results
Allegation: Failure to Observe General Infection Control Practices Specific to Respiratory PPE
The OIG substantiated that facility leaders and staff failed to observe general infection control practices specifically related to respiratory PPE.18
Infection control measures limit the spread of transmissible diseases and include wearing basic PPE, such as face masks, and more specialized items such as respirators. A 2017 VHA directive outlined policy that medical facilities would apply a combination of safe work practices, employee training, and PPE to prevent injury and illness.19 In April and May 2020, VHA issued guidance related to PPE specific to reducing transmission of COVID-19 on certain inpatient and residential units. On April 7, 2020, VHA issued a memorandum that stated “Facemasks should be used by employees working in the Community Living Center, Spinal Cord Injury units and inpatient Mental Health.”20 Face masks, when worn properly, assist in limiting the potential transmission of airborne illness.21 Nine days later, in response to concerns regarding PPE supply levels, VHA provided additional guidance stating that staff directly involved with care on CLCs will be provided one face mask or surgical mask a day to protect the residents.22 A May 1, 2020, VHA memorandum stated that “VHA staff that require additional respiratory protection to provide direct patient care (enter a room, interact within six feet) and/or evaluate any suspected or confirmed COVID-19 infected patients will receive appropriate PPE including surgical masks and/or N95 respirators or PAPRS.” Additionally, this memorandum implemented source control measures requiring the use of a face covering by all individuals entering a VHA facility and states that…“source control face coverings are to be provided to inpatients who move outside of their room.” The memorandum also notes that face coverings, most often cloth, “must cover the mouth and nose, fit snugly, and allow for breathing without restriction” and are not considered
18 The OIG considers the term respiratory PPE to refer to face coverings, face masks, N95s, and PAPRs. 19 VHA Directive 7701, Comprehensive Occupational Safety and Health Program, May 5, 2017. 20 VHA Memorandum, Updated: Coronavirus (COVID-19) Facemask and N95 Respirator Use, April 7, 2020. 21“COVID-19 Considerations for Wearing Masks,” CDC, accessed March 23, 2021,
https://web.archive.org/web/20201006013358/https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting sick/cloth-face-cover-guidance.html.
22 VHA Memorandum, Update: Coronavirus COVID-19 Return to a Contingency strategy for Facemask and N95 Respirator Use, April 16, 2020.
VA OIG 21-00553-285 | Page 9 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
PPE.23 Respirators, such as N95s or PAPRs are preferred when entering the room of a resident with known or suspected COVID-19.24
Face Coverings and Face Masks
The OIG substantiated that CLC residents did not consistently wear face coverings prior to the CLC outbreak and a few CLC staff did not comply with infection control measures related to face masks both prior to and after the CLC outbreak.25
CLC leaders and staff stated that Unity and Victory, the CLC neighborhoods that experienced the CLC outbreak in October 2020, are geri-psychiatric neighborhoods with residents who have impaired cognitive diagnoses. They also described challenges with residents wearing face coverings prior to the CLC outbreak noting compliance was complicated by the cognitive and mental disorders of CLC residents. The requirement for veterans to wear face coverings was stressed by facility and Geriatrics and Rehabilitation Service leaders during service-line meetings and town halls. At the time of the OIG’s virtual site visit in December 2020, CLC staff reported that since the CLC outbreak, compliance by residents wearing face coverings when out of their rooms had improved. During the February 2021 unannounced site visit, the residents whom OIG staff observed wore face coverings or masks when out of their rooms.
In interviews, facility and CLC leaders, the infection control coordinator, and CLC staff acknowledged that employees, including some CLC staff, did not consistently wear face masks properly. Reminders of the need to wear face masks properly were provided to staff through multiple mechanisms: CLC staff meetings and emails, facility town halls, facility-wide emails to staff, and verbally by co-workers. During the unannounced site visit, the OIG observed two employees working on a quarantined COVID-19 CLC neighborhood and wearing unapproved face coverings, or failing to cover their nose and mouth with their face mask.
The OIG team found that facility and CLC leaders took steps to emphasize and reinforce the importance of staff wearing face masks properly. The Facility Director reported supporting
23 VHA Memorandum, Update: Coronavirus (COVID-19) Mask Use in Veterans Health Administration (VHA) Facilities, May 1, 2020.
24 “Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) in Healthcare Settings,” CDC, accessed on April 22, 2021. https://stacks.cdc.gov/view/cdc/86043.
25“Interim Infection Prevention and Control Recommendations for Healthcare Personnel During the Coronavirus Disease 2019 (COVID-19) Pandemic.” Face coverings are most often cloth and are not considered PPE. “Personal Protective Equipment: Questions and Answers,” CDC, accessed on June 7, 2021.
http://web.archive.org/web/20201001160417/https://www.cdc.gov/coronavirus/2019-ncov/hcp/respirator-use faq.html. Face masks refer to non-FDA regulated procedure masks as well as surgical masks and provide barrier protection against droplets, including large respiratory particles, and are intended to prevent contamination of the surrounding area when the wearer coughs or sneezes. Fit testing is not required for face masks. Proper wearing of face masks is demonstrated when each loop is around the ears, the bendable edge of the mask is around the bridge of the nose, the mask covers the nose and mouth, and the lower edge of the mask is under the chin.
VA OIG 21-00553-285 | Page 10 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
facility supervisors taking disciplinary action for staff who were noncompliant; however, no incidents of noncompliance warranting disciplinary actions were brought to the OIG’s attention.
Respirators
The OIG substantiated that, at the time of the CLC outbreak, the facility’s Environmental and Safety Section did not identify CLC providers and nursing staff as requiring respiratory protection.26 Although not identified by the facility’s Environmental and Safety Section, the OIG found some CLC providers and one CLC nursing staff member, assigned to the impacted units, were N95fit tested.27
When caring for individuals with suspected or known cases of COVID-19, wearing respiratory protection, such as a fit tested N95 or PAPR, is key to mitigating the transmission of the virus to direct patient care providers. 28 The facility’s Environmental and Safety Section (Safety Section) is responsible for all facets of the respiratory protection program, including the development and provision of respirator training programs for N95s and PAPRs. Facility policy states that a respirator will be provided to each employee based on the need for and type of respiratory protection.29 Annually, the Safety Manager, Infection Control Coordinator, and Employee Health provider identify employees required to wear respiratory protection and then sends the list of employee names to the infection control and environment of care committees for approval. Employees must be fit tested and provided with the same make, model, style, and size of the respirator that will be used and annual testing must occur thereafter. Employees not able to wear respirators with tight fitting face-pieces will use PAPRs. Training is to consist of contaminant information, types of respiratory protection available, hands-on experience with respirators, cleaning, maintenance, and fit testing.
N95s
The Safety Manager described fit testing for N95s as a two-step process involving medical clearance from Employee Health and the fit testing session with Safety Section staff. In October 2019, staff from the Safety Section, Infection Control, and Employee Health created a memo listing the identified employees that should be included in the respiratory protection program. Although neither CLC providers or CLC nursing staff were included on the list, the Chief of Geriatrics and Rehabilitation Service discussed with the OIG about ensuring CLC providers were fit tested prior to the CLC outbreak. The OIG learned through interviews that Valor House
26 For this report the OIG considers providers to include physicians, nurse practitioners, and physician assistants. 27 Facility MCM 001ESS-11, Respiratory Protection Program, December 2017. The facility’s Respiratory Protection Program is specific to respiratory protection provided by N95s and PAPRs.
28“Interim Infection Prevention and Control Recommendations for Healthcare Personnel During the Coronavirus Disease 2019 (COVID-19) Pandemic.”
29 Facility 001ESS-11, December 2017.
VA OIG 21-00553-285 | Page 11 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
nursing staff were later identified and fit tested for N95’s in response to the possibility that the facility would use the Valor House to provide post-acute care for “stable minimally ill COVID 19 positive patients” in need of rehabilitation or as an overflow COVID-19 positive unit if the facility acute care beds were full.
The OIG learned through interviews that Unity and Victory staff did not have access to or training about respirators prior to caring for residents that tested positive for COVID-19. Therefore, staff provided direct patient care wearing surgical masks and face shields to both initial residents diagnosed with COVID-19. CLC leaders and staff confirmed that N95 fit testing for staff on Unity and Victory did not occur prior to the CLC outbreak. A revised list for fit testing was issued in December 2020, after the CLC outbreak, and included CLC providers and nursing staff. When asked about the rationale for not including CLC providers and staff on earlier lists, the Safety Manager noted the prior lack of contagious diseases in the CLC units.
During the CLC outbreak, the Safety Section was contacted by the Infection Control Coordinator and the Acting Chief Nurse of Geriatrics to request fit testing for CLC staff. The Safety Manager confirmed that after CLC providers and nursing staff were identified as requiring respiratory protection, they were to be fit tested before working with residents that tested COVID-19 positive. According to Safety Section records, none of the Unity nursing staff and one Victory nursing staff member were fit tested prior to the CLC outbreak. While CLC staff reported efforts to increase fit testing began during the CLC outbreak, the OIG learned from nursing leaders that at least three CLC nursing staff later assigned to work 101-2 were not fit tested prior to working in the unit. Safety Section records indicated 52 percent of the CLC nursing staff were fit tested as of November 23, 2020.
PAPRs
PAPRs are used to provide respiratory protection when staff are unable to tolerate N95s or when fit testing has not been completed. According to the Safety Manager, PAPRs are typically housed in the facility equipment storage warehouse and issued to the person in charge of the unit or service making the request. Reportedly, “a couple” of PAPRs were kept in the Safety Section office. A Nurse Officer on Duty (NOD) stated that part of the NOD’s duties on evenings and weekends, when the warehouse and Safety Section were closed, was to provide PAPRs for those staff who had not been fit tested for an N95. On October 19, 2020, the facility had 40 PAPRs. The Safety Manager did not know the number of PAPRs on the CLC at the time of the CLC outbreak but reported that as of December 2020, the CLC had 10.
Similar to the lack of N95 fit testing, CLC staff told the OIG that PAPR training was not provided prior to October 20, 2020, and CLC staff lacked access to PAPRs prior to CLC residents testing positive for COVID-19. Contrary to staff reports to the OIG, the NOD reported seeing PAPRs on the CLC the day the first resident tested positive for COVID-19.
VA OIG 21-00553-285 | Page 12 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
According to Safety Section records, none of the CLC nursing staff had PAPR training prior to the CLC outbreak; 6.9 percent were trained as of November 23, 2020. CLC nurse leaders told the OIG that just-in-time training about the use of PAPRs was provided to staff. However, the training was not documented and therefore, the OIG was unable to determine the extent of the training.
The OIG found the facility was compliant in 2019 and 2020 with their own policy requiring an annual review of the staff included in the respiratory protection program. However, the 2020 review was not completed until December 2020, nine months into the pandemic.
The OIG concluded that nursing leaders and the Chief of Geriatrics and Rehabilitation Service identified the need to fit test Valor House staff and CLC providers but failed to reassess the need for fit testing of other CLC nursing staff. Therefore, CLC nursing staff were not fit tested and provided N95s or trained in the use of PAPRs prior to the CLC outbreak. This failure resulted in CLC nursing staff providing direct patient care to residents with suspected and confirmed diagnoses of COVID-19 without the preferred respiratory protection.30
Allegation: Failure to Minimize Risk of Exposure to COVID-19
The OIG substantiated that CLC and facility leaders failed to minimize the risk of CLC residents and staff exposure to COVID-19. The OIG found facility leaders did not adequately respond to a CLC staff member’s reported cough and COVID-19 community close contact exposure, and did
not remove the employee from direct patient care. Additionally, the facility did not have a comprehensive plan that specified operational details such as roles, actions, and targeted time frames for the transfer and isolation of CLC residents suspected of having, or diagnosed with COVID-19. The OIG confirmed the room of a COVID-19 negative resident was cleaned after the transfer of the resident’s COVID-19 positive roommate. However, due to the non-functional bed management system and the absence of a substitute record keeping system, the OIG was unable to determine when the room was cleaned.
While not specifically referenced in the allegation, the OIG also assessed facility actions related to
∙ administering aerosol-generating procedures without infection control measures, ∙ continuing group therapy sessions, and
∙ identifying dedicated staff for the units reserved for residents with and without COVID 19.
30“Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) in Healthcare Settings.” Preferred respiratory protection for CLC staff providing care to COVID-19 infected residents include fit tested N95s or PAPRs.
VA OIG 21-00553-285 | Page 13 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
Managing Positive Staff Exposures
The OIG found facility leaders did not minimize CLC residents and staff exposure to COVID-19 when they failed to abide by VHA instructions to follow CDC guidelines. A CLC staff member reported a cough and COVID-19 community close contact exposure and was not removed from direct patient care per the guidelines.
The actions taken when an individual reports symptoms of, significant exposure to, or a diagnosis of COVID-19 are critical to limiting potential exposure to others.31 On March 6, 2020, VHA indicated that it would follow CDC guidelines.32 At the time of this event, CDC guidance stated that healthcare personnel with a known COVID-19 community close contact exposure of greater than 15 minutes should be tested and stay home until 14 days after the last exposure.33
During interviews, the OIG learned that on a morning in fall 2020, that was a federal holiday, a CLC staff member assigned to Victory had a cough and was notified, while at work, that a close family member had tested positive for COVID-19. The CLC staff member then notified a colleague about the exposure. Information as to what occurred next was conflicting. A few interviewees reported that the notification went through the chain of command and ultimately the Acting ADPCS was contacted and gave instructions that the CLC staff member would not be tested, should wear a mask, and continue to work, providing direct patient care for the remaining six hours of the shift. Contrary to these reports, the Acting ADPCS stated having no knowledge of this event. The staff member recalled being told no when asking for a COVID-19 test and to put a mask on and continue working.
The CLC staff member stated that the following day, the Chief of Geriatrics and Rehabilitation Service arranged for testing and was called at home by co-workers and told to come into the facility.34 The staff member reported not working that day, being tested at the facility’s urgent care at approximately 8:30 a.m., and being notified of a positive test result around 1:00 p.m. Employee Health contacted the CLC staff member and advised to quarantine based on CDC guidelines.
CLC nurse managers stated that Employee Health would be contacted if there was concern that a staff member was exposed or had COVID-19 symptoms. However, since the day was a federal holiday, Employee Health staff were not available for consultation and the Acting ADPCS was
31“Public Health Guidance for Community-Related Exposure,” CDC, accessed on December 30, 2020, https://www.cdc.gov/coronavirus/2019-ncov/php/public-health.recommendations.html.
32 VHA, COVID-19 Communications Toolkit, March 6, 2020.
33 “Public Health Guidance for Community-Related Exposure;” “Interim Guidance on Testing Healthcare Personnel for SARS-CoV-2,” CDC, accessed on October 2, 2020, https://www.cdc.gov/coronavirus/2019-ncov/hcp/testing healthcare-personnel.html. On March 10, 2021, CDC updated guidance states that asymptomatic healthcare personnel who are fully vaccinated do not have to be restricted from work.
34 The CLC staff member stated being unsuccessful when attempting to receive a COVID-19 test in the community.
VA OIG 21-00553-285 | Page 14 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
called for guidance.35 CLC nurse managers stated although they did not think the CLC staff member should stay on duty, they followed the guidance of the Acting ADPCS.
An Employee Health provider told the OIG that in addition to all-employee emails and availability via telephone, a decision tree following CDC guidelines was developed to serve as the main source of guidance for staff questions related to exposure and symptoms for COVID 19. The OIG reviewed the decision tree and found that it was not created until December 8, 2020.
The OIG concluded facility and CLC leaders did not adhere to VHA instructions to follow CDC guidance for removing a CLC staff member with a cough and a known COVID-19 community close contact exposure from duty.36 This failure resulted in an employee, who later tested positive for COVID-19, providing direct patient care and potentially exposing CLC residents and staff to COVID-19.
Resident Transfers and Isolation
The OIG determined that the facility did not have a comprehensive plan to address the transfer and isolation of CLC residents suspected of having, or diagnosed with, COVID-19. While the facility did develop a surge plan, it was not finalized until after CLC residents were diagnosed with COVID-19 and lacked specific operational details such as roles, actions, and targeted time frames.
At the beginning of the CLC outbreak, two CLC residents (resident A and resident B) were diagnosed with COVID-19, one of whom (resident B) lived in a shared room. The OIG found that resident B’s non-infected roommate (resident C) was not isolated.
Isolating individuals with known exposure to, or a confirmed diagnosis of, COVID-19 reduces the likelihood of transmission to others. VHA guidance for CLCs dated March 17, 2020, stated, “the facility should have a plan to isolate a resident that is suspected of having COVID-19.” The guidance further stated, “Facilities with multiple suspected or confirmed cases should have plans to isolate residents to one area (neighborhood) in the CLC or at another location at the medical center if space does not allow to isolate in the CLC.”37 The VHA guidance was not prescriptive regarding time frames for relocating residents with suspected or confirmed COVID-19.38
35 Employee Health hours of operation are Monday–Friday, 8:00 a.m. to 4:30 p.m.
36 In February 2021 during a follow-up interview, the OIG informed the Facility Director about the CLC staff member’s exposure. The Facility Director was not aware of the exposure and subsequently initiated a fact-finding; however, the fact-finding was inconclusive due to conflicting testimony and the Facility Director is evaluating next steps.
37 VHA Memorandum, Coronavirus (COVID-19) Community Living Centers-Revised 03/17/2020. 38 VHA Memorandum, Coronavirus (COVID-19) Community Living Centers-Revised 03/17/2020.
VA OIG 21-00553-285 | Page 15 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
VHA guidance defers to each facility to determine the specifics related to managing the transfer and isolation of residents suspected of having, or diagnosed with, COVID-19.39 The plan developed by the facility was finalized after the CLC outbreak started and did not provide staff with the necessary specifications to carry out the task. The OIG was unable to determine if facility leaders had requested clarification on the VHA guidance regarding the required time frame to transfer a patient after notification of a positive COVID-19 test result to assist them with development of the plan.
For further clarification on the expected time frame to relocate a resident suspected of having, or diagnosed with, COVID-19 and how to manage a roommate who is COVID-19 negative, the OIG contacted VHA’s Office of Patient Care Services. The response, approved by the VHA Acting Principal Deputy Under Secretary for Health, stated, “Veteran is cohorted from the COVID negative Veteran to prevent cross-transmission…The time frame to relocate the CLC resident to the designated COVID area should occur upon identification of the resident’s COVID status. The COVID negative resident will continue to be monitored as required.”
During interviews, the OIG learned that on the date at issue, resident A lived in a private room and resident B shared a room with resident C, who was known by CLC staff to walk around the neighborhood. The EHR reflected that at 9:10 p.m., the lab notified the after-hours physician of positive COVID-19 results for resident A and resident B. Between 9:25 p.m. and 10:02 p.m., the physician notified a CLC nurse of the lab results. The OIG learned through EHR documentation and an interview with a nursing staff member, that the nurse informed the NOD of the positive lab results, discussed concerns regarding the cohabitation of resident B and resident C, and awaited further instruction from the NOD regarding resident B. Later that evening, the off-tour CLC physician and NOD came to the unit to assess the status of both residents. In the absence of local guidance, the off-tour CLC physician determined that resident A could remain in the private room. Resident B was approved to stay overnight in the room with resident C, the COVID-19 negative roommate, since resident C had already been exposed.
EHR documentation and interviews with CLC staff indicated both nursing and medical staff anticipated transferring residents A and B to Valor House around 7:45 a.m. the day following the positive COVID-19 results. A CLC staff member told the OIG that around 7:30 a.m., the transfer was postponed until 1:30 p.m. citing transportation issues. The staff member also reported a lack of direction regarding which staff should care for the residents diagnosed with COVID-19 and which isolation protocols to use for the COVID-19 positive resident sharing a room. Staff told the OIG that during this period, resident C paced the neighborhood, including communal areas where other residents were congregated. Staff also gave conflicting information on whether resident C was wearing a face covering while walking around the neighborhood.
39 VHA Memorandum, Coronavirus (COVID-19) Community Living Centers - Revised 03/17/2020.
VA OIG 21-00553-285 | Page 16 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
The transfers for residents A and B were further delayed due to a change in the transfer location. Per the Acting ADPCS, the residents would move to unit 101-2 later that day because Valor House was nearing capacity. At 5:45 p.m., CLC staff received authorization and moved both residents to unit 101-2. The transfer occurred 20 hours after the physician first became aware of both residents’ positive COVID-19 tests. Of note, after several COVID-19 negative test results, resident C tested positive for COVID-19 (14 days after the roommate’s positive result) and was transferred to 101-2 without delay. Although the OIG could not determine that resident C contracting COVID-19 was a consequence of being left in a room with the COVID-19 positive roommate, the lack of a plan to isolate residents was likely a contributory factor.
Room Disinfection
The OIG confirmed that resident C’s room was cleaned after the transfer of the COVID-19 positive roommate; however, due to a lack of record keeping, the OIG was unable to determine the time of the cleaning. The OIG did not assess the cleaning status of the single occupant room of resident A because the timing of the cleaning did not impact a roommate.
Cleaning spaces occupied by individuals with COVID-19 prevents potential transmission of the disease, through contaminated surfaces, to future occupants of the space.40 VHA guidance indicates that the bed management system should be updated as part of the discharge or transfer cleaning process for a patient’s room to ensure proper bed flow data.41 A March 2020 facility SOP outlined the proper and safe cleaning techniques to disinfect a room that has housed an individual with suspected or confirmed COVID-19.42
A CLC staff member reported to the OIG that prior to the transfer of residents A and B, Environmental Management Service staff brought cleaning supplies to the unit at 1:30 p.m. but were unable to clean the room at that time because the transfer of resident A and B had been further delayed. Once the two residents transferred, a CLC staff member requested cleaning of the rooms. The staff member conveyed that at 5:45 p.m. the Environmental Management Service supervisor on duty was notified that the shared room had not been cleaned to allow resident C to continue residing in the room. The same CLC staff member did not know when the room was cleaned, but reported receiving a text while at home from a colleague on duty indicating the room was cleaned. The OIG learned there were no complaints elevated to Environmental Management Service leaders by CLC staff regarding room cleaning delays on October 21, the day the cleaning occurred.
40“Guidance for Cleaning and Disinfecting Public Spaces, Workplaces, Businesses, Schools, and Homes,” CDC, accessed March 23, 2021, https://www.cdc.gov/coronavirus/2019-
ncov/community/pdf/REopening_America_Guidance.pdf.
41 VHA, Environmental Management Services, Sanitation Procedural Guide, 2016.
42 Facility Environmental Management Service, Standard Operating Procedure No 47-137, March 2020.
VA OIG 21-00553-285 | Page 17 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
According to the Chief of Environmental Management Service, a housekeeper is assigned to the CLC during the first shift but not the second or third shift.43 Per the Chief of Environmental Management Service and an Environmental Management Service staff member, the response time for cleaning at the CLC is 30 minutes or less. When the OIG inquired about mechanisms to track room cleaning, the Environmental Management Chief reported that the bed management system used to track discharge cleanings was not operational and an alternative system of record keeping was not in place. A verbal hand-off between staff was used to communicate bed cleaning status despite the procedural guide directing staff to document room cleaning in the bed management system.44
Due to an inoperable bed management system and the lack of an alternative system of record keeping, the OIG was unable to determine when the cleaning of the room was initiated and completed following the transfer of resident B.
Aerosol-Generating Procedures
The OIG determined that facility and CLC leaders did not implement the additional infection control measures recommended by the CDC when administering aerosol-generating procedures.
COVID-19 is a virus transmitted through respiratory droplets.45 The CDC explains that some procedures performed on patients with suspected or diagnosed COVID-19 could produce infected aerosols. When procedures that pose such risk cannot be avoided, staff should perform procedures cautiously with additional infection control measures including
∙ wearing an N95 or PAPR, a face shield or goggles, gloves, and a gown, ∙ limiting the number of staff present during the procedure,
∙ administering the procedure in a negative pressure room whenever possible,
∙ keeping doors closed except when entering or leaving the room, which should be minimized and,
∙ disinfecting a room soon after completion of the procedure.46
VHA guidance confirms that nebulizer treatments and continuous positive airway pressure (CPAP) are classified as aerosol-generating procedures. The guidance further states that when a patient has not been COVID-19 tested in the past 72 hours, or has results pending, they should be
43 The facility provided the following for shift descriptions: 7:00 a.m.-3:30 p.m. (first shift), 3:30 p.m.–12:00 a.m. (second shift), and 10:00 p.m.–6:30 a.m. (third shift).
44 VHA, Environmental Management Services, Sanitation Procedural Guide, 2016.
45“How Coronavirus Spreads,” CDC, accessed April 12, 2021, https://www.cdc.gov/coronavirus/2019- ncov/prevent-getting-sick/how-covid-spreads.html.
46“Interim Infection Prevention and Control Recommendations for Healthcare Personnel During the Coronavirus Disease 2019 (COVID-19) Pandemic.”
VA OIG 21-00553-285 | Page 18 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
treated as COVID-19-positive when performing procedures that have a high risk of transmission.47
The OIG conducted an EHR review of residents residing in the CLC who were prescribed an aerosol-generating procedure (nebulizer or CPAP) during the time frame of the CLC outbreak. The OIG found two residents that were receiving aerosol-generated procedures and reviewed
their care. Neither resident was being tested for COVID-19 every 72 hours, therefore, additional infection control measures should have been used during administration. Both residents became COVID-19 positive during the CLC outbreak.
In an interview with the OIG, the Chief of Geriatrics and Rehabilitation Service reported being unaware of nebulizer use at the CLC during the COVID-19 pandemic and stated that if a resident needed a nebulizer, they would be transferred to the acute inpatient unit to have it administered in a negative pressure room. The OIG learned that facility leaders had not discussed additional infection control measures, recommended for aerosol-generating procedures, until early December 2020 after a respiratory therapist brought concerns of nebulizer and CPAP use without proper infection control precautions to the attention of facility leaders and the infection control coordinator. As a result, a nurse who provided nebulizer treatments reported being unaware of special precautions related to aerosol-generating procedures for residents who were not recently tested, were suspected to have, or known to have, a COVID-19 positive diagnosis. The nurse reported administering the nebulizer in the resident’s room wearing a gown, gloves, and a surgical mask prior to the December discussion. Had staff been familiar with the precautions, there were still impediments; none of the CLC nursing staff had been trained on the use of a PAPR, and only 5 percent had been N95 fit tested at the start of the CLC outbreak.
The OIG determined that the failure of CLC leaders to disseminate information regarding the implementation of additional infection control measures to limit CLC residents and staff exposure to COVID-19 during aerosol-generating procedures throughout the pandemic resulted in noncompliance with VHA and CDC guidance.
Group Therapies
The OIG team found CLC leaders permitted group therapy sessions to continue throughout the pandemic thereby increasing residents and staff risk of exposure to COVID-19.
CLCs are residents’ home. As such, the availability of purposeful activity is an important part of the environment. To increase socialization and reduce isolation, activities are often provided in group settings. In response to the risks associated with transmission of COVID-19, a March 17, 2020, VHA memorandum stated that facilities with CLCs should immediately initiate procedures
47 VHA, Moving Forward Together, Guidance for Resumption of Procedures for Non-Urgent and Elective Indications, ver 2.0, August 19, 2020.
VA OIG 21-00553-285 | Page 19 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
to cancel all group activities.48 In an interview with the National Program Director of Recreation Therapy, the OIG learned that while there was some flexibility to vary from the guidance provided to the field, the expectation was that a facility director be involved with making that decision.
Through a review of EHR records, the OIG found CLC residents attended group therapy sessions during the CLC outbreak. Facility documents show that CLC residents attended multiple group sessions prior to, during, and after the main CLC outbreak. In reviewing these documents, along with EHR records, the OIG identified that two Unity residents tested positive for COVID-19 the same day after they attended separate group therapy sessions with five other residents. Similarly, three of the first four Victory residents diagnosed with COVID-19 attended a group therapy session three days earlier with six other residents. When speaking with CLC staff, the OIG was told that prior to the CLC outbreak, the facilitator wore a face mask during these group sessions; however, the residents did not.
The Facility Director, Acting Chief of Staff, and Acting ADPCS reported awareness of the VHA guidance to stop all group activities. The Acting Chief of Staff and Acting ADPCS indicated that they were not aware of CLC group therapy sessions taking place throughout the pandemic. The Chief of Geriatrics and Rehabilitation Service sent an email on April 3, 2020, to service line and recreation therapy staff with the March 17, 2020, memo attached. The email stated, “regarding groups, there is no clear-cut guidance whether “groups” can occur…it is my understanding that we should not have more than 10 people, including staff, in one area at once and all should be at least 6 feet apart.” Additionally, the Chief of Geriatrics and Rehabilitation Service reported in an email to the OIG that all CLC group activities were suspended after the March 17, 2020, VHA guidance was released.49 In interviews with the OIG, recreation therapists and a CLC leader indicated that they had not been made aware of the VHA guidance to stop all group therapies. A recreation therapist stated that guidance and information on COVID-19 would come from the service chief, in this case the Chief of Geriatrics and Rehabilitation Service. Recreation therapists described their concern for both the physical and emotional well-being of the CLC residents and shared they wanted to do the best they could with the information that they had.
The OIG concluded that facility leaders were aware of VHA guidance to stop all group activities at the CLC. However, facility leaders were not involved in the decision-making to continue the group activities and were not aware they were occurring. The statement from the Chief of Geriatrics and Rehabilitation Service that group activities were not taking place in the CLC during the COVID-19 pandemic is inconsistent with evidence obtained by the OIG. Continuation of group therapy sessions during the pandemic increased the risk of exposure to COVID-19 for
48 VHA Memorandum, Coronavirus (COVID-19) Community Living Centers – Revised 03/17/2020. 49 VHA Memorandum, Coronavirus (COVID-19) Community Living Centers – Revised 03/17/2020.
VA OIG 21-00553-285 | Page 20 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
CLC residents and staff and is indicative of a failure by CLC leaders to understand, communicate, and implement VHA guidance.
Nurse Staffing Assignments
The OIG determined facility leaders minimized the risk of cross-contamination by ensuring staff did not work on both the non-COVID-19 and COVID-19 units during the same work shift.
Given minimal movement of residents off the CLC, employees posed the greatest risk to residents for exposure to COVID-19. The March 17, 2020, VHA memorandum stated, “if the need to isolate in a neighborhood setting is required, consistent staff should be assigned to those residents and not be assigned to go between COVID-19 infected and negative residents to provide care.”50 The OIG reached out to VHA’s Office of Patient Care Services for clarification whether staff movement between COVID-19 positive and negative units should be limited to within a shift or day to day. The written response stated, “staff movement (assignment) is to be limited within a shift to prevent cross-transmission from COVID-19 positive to negative residents….”51
During interviews with the OIG, CLC nursing staff expressed concern with nurses working on both 101-1 (non-COVID-19) and 101-2 (COVID-19), and sharing a common hallway and restroom. A review conducted by the OIG of CLC nursing staff assignments on 101-1 and 101-2 from October 25 through November 13, 2020, found 11 nursing staff members were assigned to work shifts on both units, but on different days. There were three occurrences of nursing staff members assigned to work shifts on both units on the same day; however, there were no instances of nursing staff assigned to work both units during the same shift.
During the virtual tour of units 101-1 and 101-2 and the on-site visit, the OIG saw the common hallway with two restrooms. The OIG observed signage on each restroom designating the use for either 101-1 or 101-2 staff, respectively.
Ancillary service staff not solely assigned to a single CLC unit reported a combination of approaches to mitigate risk of COVID-19 exposure while providing care on multiple units throughout a shift. Approaches to mitigating risk included: using PPE, social distancing, and scheduling non-COVID-19 care prior to seeing residents diagnosed with COVID-19.
The OIG found that CLC leaders minimized the risk of cross-contamination by ensuring staff did not work on both the non-COVID-19 and COVID-19 designated units during the same shift.
50 VHA Memorandum, Coronavirus (COVID-19) Community Living Centers - Revised 03/17/2020. 51 VHA Memorandum, Coronavirus (COVID-19) Community Living Centers - Revised 03/17/2020.
VA OIG 21-00553-285 | Page 21 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
Allegation: Inconsistent Ongoing Testing and Failure to Notify of Positive COVID-19 Test Results
The OIG found the facility lacked a plan for post-baseline testing of residents and staff. Additionally, the OIG substantiated that ongoing testing for residents and staff was inconsistent following the CLC outbreak. The OIG did not substantiate that the facility failed to notify residents, their families, and staff of COVID-19 test results.
Inadequate Post-Baseline Testing Plan
While reviewing the facility process to test residents and staff for COVID-19, the OIG determined that the facility plan for COVID-19 post-baseline testing for the CLC was not in accordance with VHA guidance.
Testing for COVID-19 provides facility staff with information regarding disease activity among CLC residents and staff.52 In April 2020, VHA released specific testing guidance for CLCs and Spinal Cord Injury and Disorder units that stated each facility director “should develop a plan for ongoing COVID-19 disease screening, monitoring, and testing for Veterans/residents and employees in CLCs and SCI/D [Spinal Cord Injury and Disorder] units once baseline testing is completed.”53 Similarly, the CDC guided facilities to put a testing plan in place to identify (1) triggers for when to perform testing, (2) the process that will be taken to perform testing on all residents and staff, and (3) how residents and staff who refuse or are unable to be tested will be addressed.54
When the OIG requested the required COVID-19 testing plan, a facility staff member provided a facility SOP outlining the step-by-step process for performing CLC resident and staff testing, and actions to take based on test results. The SOP lacked a plan for ongoing screening, monitoring, and the frequency of testing.55 The staff member also provided the March 2020 guidance from VHA as evidence of a plan for screening and monitoring.56 This document was released more than a month before VHA required facilities to create a post-baseline testing plan and provided guidance on multiple topics but was not a plan for screening, monitoring, or testing. The OIG noted that the facility SOP dated April 2020 did not follow the March 2020 VHA guidance encouraging facilities to have CLC nursing staff perform all duties within their scope of practice
52 VHA Memorandum, COVID-19 Guidance on COVID-19 Testing for Community Living Centers and Spinal Cord Injury and Disorder Units, June 11, 2020.
53 VHA Memorandum, Coronavirus (COVID-19) Community Living Center (CLC) and Spinal Cord Injury and Disorder Unit (SCI/D) Veteran and Staff Testing, April 14, 2020.
54“Preparing for COVID-19 in Nursing Homes,” CDC, accessed February 11, 2021
https://www.cdc.gov/coronavirus/2019-ncov/hcp/long-term-care.html.
55 Facility Community Living Center Standard Operating Procedure, COVID-19 Testing Residents/Staff, April 4, 2020.
56 VA Response to COVID-19, Guidance for VA Community Living Centers, March 6, 2020.
VA OIG 21-00553-285 | Page 22 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
in an attempt to limit the number of staff entering the CLC. Instead, the facility SOP relied on urgent care and acute nursing staff to administer the COVID-19 tests.57
The importance of COVID-19 testing cannot be understated, without it, silent transmission can occur due to the risk of an infected person being asymptomatic.58 An Employee Health provider, the infection control coordinator, nursing leaders, and staff reported that before the CLC outbreak, residents and staff were to be tested monthly; however, staff reported that they were not tested consistently. An Employee Health provider and the infection control coordinator told the OIG that the determination to test residents and staff monthly was made at the command center level and shared with staff. However, the OIG did not find evidence to support that the command center team made the decision or communicated the information to staff.
The OIG found facility leaders did not create an adequate COVID-19 post-baseline testing plan; this resulted in the lack of a standardized process to address ongoing disease screening, monitoring, and testing of CLC residents and staff for the prevalence of COVID-19.
Inconsistent Ongoing Testing Following a COVID-19 Outbreak
The OIG substantiated that although CLC residents were tested, facility leaders failed to ensure testing of all CLC staff after an individual at the CLC was diagnosed with COVID-19.
When outbreaks of COVID-19 occur, routine testing to identify individuals with the virus is critical to limit the spread of the disease. A June 11, 2020, VHA memorandum states all CLC residents and staff should be tested as soon as a newly confirmed case of COVID-19 is identified. The same memorandum further instructs facilities to, “continue to test residents and staff who initially test negative weekly until no new cases are identified and at least 14 days have passed since the most recent positive test in the unit.”59
Following the CLC staff member’s positive COVID-19 test on October 13, 2020, per VHA guidance, all CLC residents and staff should have been tested for COVID-19 as soon as possible.60 The OIG reviewed the EHR and facility databases for COVID-19 testing of CLC residents and staff for the week after the CLC staff member tested positive. The OIG found that 67 percent of Victory and 22 percent of Unity staff were tested on their next shift back to work. Three Victory and two Unity staff worked multiple shifts between October 13–19, 2020, before testing occurred and ultimately tested positive. The OIG found that by October 14, 2020, COVID-19 testing was complete for all residents on CLC neighborhoods Victory and Unity.
57 Facility Community Living Center, COVID-19 Testing, April 4, 2020.
58“Why COVID-19 is The Key to Getting Back to Normal,” National Institute of Health, September 04, 2020 https://www.nia.nih.gov/news/why-covid-19-testing-key-getting-back-normal.
59 VHA Memorandum, COVID-19 Guidance on COVID-19 Testing for Community Living Centers and Spinal Cord. 60 VHA Memorandum, COVID-19 Guidance on COVID-19 Testing for Community Living Centers and Spinal Cord.
VA OIG 21-00553-285 | Page 23 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
In addition to the immediate testing for COVID-19, CLC residents and staff who initially tested negative should have been retested weekly and until 14 days had passed after the most recent positive test. The OIG learned through interviews with CLC staff that resident and staff testing for COVID-19 increased following the identification of residents and staff diagnosed with COVID-19; however, the frequency was inconsistent. The OIG verified the frequency of resident and staff testing for the duration of the CLC outbreak through a review of documentation provided by the facility and in the EHR. Table 2 shows the weekly testing compliance rates for CLC residents and staff on Unity and Victory for the duration of the CLC outbreak. 61
Table 2. Weekly Testing Completion Rates for Residents and Staff on Unity and Victory for the Duration of the CLC Outbreak
| Week 1 | Week 2 | Week 3 | Week 4 |
| 100% | 100% | 100% | 100% |
| 100% | 100% | 100% | 33% |
| 41% | 74% | 37% | 71% |
| 100% | 35% | 31% | 20% |
Testing Group Week 5 Unity Residents 100% Victory Residents 67% Unity Staff 7% Victory Staff 27% Source: OIG analysis of EHRs and data provided by Employee Health.
The OIG found through interviews with Employee Health, nursing leaders, and staff, that there was no formalized process for tracking weekly COVID-19 testing of residents and staff. The Chief of Geriatric and Rehabilitation Service reported that residents were tested weekly and an administrative staff member maintained a grid that tracked resident testing. Employee Health and nurse leaders told the OIG that nurse supervisors were responsible for ensuring 100 percent compliance with staff testing. A CLC nurse leader described a process in which paper lab requisition forms would be printed and staff would be marked off once they were tested by one of three CLC nurses identified as unit COVID-19 champions. These forms were shredded when no longer in use. While the OIG learned of this process through interviews, this process was not included in the CLC testing SOP.62 The SOP outlined the process for testing residents and staff as well as actions to take depending on results. However, the SOP did not state the frequency to conduct testing or specify roles and responsibilities regarding processes and accountability for ensuring all staff were tested. CLC nurse leaders recognized that 100 percent COVID-19 testing compliance did not occur and attributed it to staff schedules, leave status, and confusion over whether the testing was mandatory.
61 The OIG did not include staff members and residents who had already tested positive for COVID-19 in subsequent weekly data as the CDC recommends that diagnostic testing for COVID-19 does not resume for three months after the date of initial symptom onset. The OIG did not include staff in a leave status in data for time periods because they were not available for testing.
62 Facility Community Living Center SOP, COVID-19 Testing Residents/Staff.
VA OIG 21-00553-285 | Page 24 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
The OIG found that the failure to test all CLC staff during their first shift after a known positive test result may have led to staff members working while having COVID-19. Additionally, the OIG found that facility leaders did not implement a reliable method of tracking weekly testing for CLC residents and staff during the CLC outbreak. A lack of clear roles and responsibilities outlined in an SOP likely led to confusion as to who was responsible for ensuring testing occurred and the failure to test all residents and staff as required. Missed testing represents a missed opportunity to promptly identify and isolate residents and staff diagnosed with COVID 19 to reduce further transmission of the virus.
Notification of COVID-19 Test Results
The OIG did not substantiate a failure to notify residents, their families, and staff of positive COVID-19 test results. The OIG found that the facility had a process in place to manage communication of staff members’ positive COVID-19 test results within the supervisory structure. Additionally, although staff could not articulate the individual responsible for notifying residents or their family of a residents positive COVID-19 test result, documentation in the EHR showed notification occurred.
Contact tracing is the process of notifying individuals who have been in contact with someone who tests positive for COVID-19; it is an infection control practice intended to stop or slow the spread of further transmission. The act of quarantining keeps individuals exposed to the virus away from others.63
Resident
The OIG found that CLC staff were unable to verbalize who was responsible for notifying a resident or point of contact (POC) when a resident had a positive COVID-19 test result. This was despite evidence that notification of a resident’s COVID-19 diagnosis, and subsequent change of room location occurred and was made by nursing staff.
The CLC COVID-19 SOP on testing residents and staff specifies, “Resident POC [Point of Contact] will be notified of the testing if deemed incompetent to make medical decisions” and “If the test comes back positive Resident (POC) will be informed of the positive test results.”64 However, the SOP does not state who is responsible for notifying the resident or the POC of a positive test result.
63“Isolate if You are Sick,” CDC, accessed on March 23, 2021, https://www.cdc.gov/coronavirus/2019-ncov/if-you are-sick/isolation.html.
64 Facility Community Living Center SOP, COVID-19 Testing Residents/Staff. This SOP uses the acronym POC, which stands for point of contact.
VA OIG 21-00553-285 | Page 25 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
According to a July 2018 facility nursing SOP, nursing staff are to document patient transfers using the NUR/TRANSFER NOTE in the EHR. The note should include the reason for transfer, notification of next of kin, and by whom.65
The OIG interviewed facility and CLC leaders and CLC staff regarding who was responsible for notifying the resident and or their POC of a resident’s testing and positive COVID-19 test result. The responses were inconsistent but commonly attributed the responsibility to physicians, nurse
practitioners, and nursing staff. The OIG reviewed the EHRs of 23 Unity and Victory residents diagnosed with COVID-19 and found that all 23 POCs were notified of the resident’s COVID-19 positive test result and relocation to the designated treatment unit. Additionally, the OIG found that nursing staff provided the notification to POCs.
The OIG concluded that although CLC staff were unable to verbalize the person responsible for notifying the resident and or their POC of a resident’s positive COVID-19 test result, nursing staff completed the notifications to residents or their POC.
Staff
The facility had a process to inform supervisors of an employee’s positive COVID-19 test result and to alert staff of possible exposure in a manner that protected the affected individual’s confidentiality.
An April 3, 2020, VHA memorandum explains that contact tracing and risk-assessment of all potentially exposed health care personnel is costly to resources and impractical in areas with community transmission, citing that when community transmission is high, healthcare workers are assumed to be at high risk of exposure. Therefore, because the use of formal contact tracing may place an undue demand on the system and unnecessarily pull resources from elsewhere, VHA recommends that healthcare workers report significant exposures, self-monitor, and stay home if ill.66 On June 18, 2020, the CDC issued guidance that stated when informing individuals of exposure to COVID-19, notification should “be carried out in a way that protects the confidentiality of affected individuals and is consistent with applicable laws and regulations.”67
Through interviews and a review of the facility’s COVID-19 employee databases, the OIG learned of a facility process to notify supervisors of a staff member’s positive COVID-19 test result and alert staff of a possible workplace-related exposure. Employee Health maintains a database of persons under investigation, defined by an Employee Health provider as a staff member falling into one of three categories: tested at the facility, tested in the community, or
65 Facility SOP 118-6, Nursing Documentation, July 2018.
66 VHA Memorandum, Guidance for Notification Surrounding Exposure to Health Care Personnel (HCP) with Confirmed 2019 Novel Coronavirus (COVID-19) Illness, April 3, 2020.
67“Interim Infection Prevention and Control Recommendations for Healthcare Personnel During the Coronavirus Disease 2019 (COVID-19) Pandemic.”
VA OIG 21-00553-285 | Page 26 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
self-isolated at home due to a positive family member. At the time of the inspection, persons under investigation could receive a COVID-19 test either at the facility or within the community. The OIG was told that regardless of test location, staff were advised to inform their supervisor about the potential exposure, plan for testing, and need to quarantine until the final test results were known. Information including the name of the COVID-19 positive staff member, duration of quarantine, and the return to work date was maintained within the database. When results were known, Employee Health sent an email to the supervisor regarding the COVID-19 positive staff member to inform them that one of their staff tested positive. Additionally, Employee Health sent a separate email for supervisors to forward to staff telling them someone had tested positive in their work area while protecting the identity of the positive staff member, in accordance with CDC guidance. As a staff member reached the end of their quarantine period, Employee Health contacted them to check on their condition and discuss release from quarantine. Once ready to return to work, the staff member was asked to contact their supervisor to finalize the date of return.68 Employee Health provided a daily report on the number of individuals who had tested positive or who were under investigation to the command center and the Chief Nurse of Operations.
The OIG found processes in place at the facility that adhered with guidance for informing supervisors and staff of positive COVID-19 results in a manner that protected confidentiality.
Contributory Factors
The OIG team identified a failure by facility leaders to proactively develop and implement plans to prepare for, and respond to, a potential COVID-19 outbreak at the CLC following VHA’s identification of the CLC as a high-risk environment.69 The OIG found the facility’s initial action plan, prepared prior to the official recognition of the pandemic and inception of the command center, lacked planning specific to CLC preparedness for mitigating or responding to COVID-19. Rather, the Facility Director stated focusing on planning for an influx of VHA patients from other geographic regions or non-VHA patients from the community who may have needed to be quarantined at the facility due to a lack of beds elsewhere.
Early in the pandemic, due to their high-risk population, VHA identified CLCs as locations that warranted special precautions to mitigate exposure to and transmission of COVID-19.70 The Chief of Quality Management reported the facility created an action plan in response to pandemic-related actions assigned to medical centers by VHA’s Deputy Under Secretary for Health for Operations and Management. Later, facility leaders contributed to the development of the plan. In total the plan included 46 items, only two were specific to the CLC. The first was a
68“Interim Infection Prevention and Control Recommendations for Healthcare Personnel During the Coronavirus Disease 2019 (COVID-19 Pandemic.”
69 VA Response to COVID-19, Guidance for VA Community Living Centers.
70 VA Response to COVID-19, Guidance for VA Community Living Centers.
VA OIG 21-00553-285 | Page 27 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
response to queries regarding the availability of space to provide a mobile hospital and staff to provide training. The second focused on screening individuals entering the CLC. The plan lacked items specific to a potential outbreak at the CLC.
The OIG learned through interviews that staffing of the command center, that opened on March 23, 2020, included facility leaders, the Chiefs of Quality Management and Environmental Management Service, the emergency manager, and the infection control coordinator. CLC leaders were not members of the command center. Command center members met together at least weekly from March 23, 2020, until the command center transitioned to virtual meetings in June 2020.
The Facility Director stated plans were initiated in March 2020 to address how the facility would manage VHA patients from other geographic regions or non-VHA patients from the community who may have needed to be quarantined. Units 101-1 and 101-2 were designated for the anticipated quarantined patients. The Facility Director acknowledged that an internal outbreak was not part of the considerations.
The Facility Director told the OIG that after a neighborhood-wide testing occurred on October 20, 2020, two residents at the main CLC tested positive and that the Director met with the Associate Director, Chief of Staff, and ADPCS to determine next steps; at that time, two CLC neighborhoods, 101-1 and 101-2, and Valor House were vacant. The Director stated that “in an attempt to move out with a sense of urgency to mitigate this on a wider scale” a decision was made to separate the residents and use 101-1 for residents who were not diagnosed with COVID 19 and 101-2 for residents diagnosed with COVID-19. The decision was shared with representatives from the CLC and other service lines. The OIG confirmed 101-2 opened on October 21, 2020, and the two residents diagnosed with COVID-19 were moved to the unit the same day.
The CLC outbreak led to completion of a facility inpatient surge plan on October 22, 2020. The surge plan addressed bed management and had three stages specific to the placement of patients diagnosed with COVID-19 (see appendix B):
∙ Utilize the two negative pressure rooms on an inpatient medical unit,
∙ Activate Valor House when the census reaches three, and
∙ Activate 101-2 when the census reaches 10.
The remaining residents were retested on October 23, 2020. On October 24, 2020, unit 101-1 opened; CLC residents who remained negative for COVID-19 transferred to the unit. From late March until October 2020, when community spread was at low levels, facility leaders had the opportunity to put processes and plans in place to mitigate and manage a potential COVID- 19 outbreak at the CLC. The initial focus of facility leaders on plans to receive and care for patients from the community and other VHA facilities, coupled with the initial level of community
VA OIG 21-00553-285 | Page 28 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
spread, may have contributed to a lack of urgency and lack of planning for the possible need to provide care to significant numbers of CLC residents diagnosed with COVID-19 at the facility.
The OIG team identified the lack of CLC-specific planning as a contributory factor that led to a failure to: identify CLC staff as requiring respiratory protection, being fit tested and issued N95s, and trained in the use of PAPRs; develop thorough processes to minimize exposure; and ensure consistent testing for residents and staff. Despite clear communication from VHA emphasizing the need to pay particular attention to CLCs, facility leaders did not initiate CLC-specific planning until the CLC outbreak occurred, seven months into the pandemic. This failure to proactively develop and implement plans was a missed opportunity to ensure that facility and CLC staff were in a state of ongoing readiness should a CLC resident or staff member become diagnosed with COVID-19.
Concern: Facility and CLC Leaders’ Post-CLC Outbreak Actions
The OIG determined that actions taken by facility and CLC leaders following the CLC outbreak lacked input from frontline staff to identify corrective actions and opportunities for improvement. However, the facility has made significant progress toward mitigation of the spread through vaccines.
The OIG team asked facility and CLC leaders, as well as staff, to reflect on the CLC outbreak and the level of readiness for a similar event, were one to occur. The OIG heard starkly different responses. One facility leader described the time frame during the CLC outbreak as difficult, not because the information about COVID-19 was still changing but because they were having to apply it for the first time, months after the pandemic started. Overall, facility leaders reported pride in the facility’s response, felt confident in their readiness to handle possible future outbreaks, and that staff understood actions to take were that to occur. CLC managers and direct care staff reported feeling they could have been better prepared for the CLC outbreak and lacked confidence in their readiness to respond to subsequent COVID-19-related challenges. Direct care staff described chaos and a lack of awareness of what to do once the CLC outbreak occurred. They reported doing their best with little recent training or experience to draw upon.
On October 22, 2020, in response to the CLC outbreak, CLC leaders finalized an upsurge action plan. The action items focused on CLC staff education about PPE and auditing of correct PPE use. The plan addressed proper face mask wearing education, both face-to-face and computerized training modules, weekly audits of five staff members to monitor compliance, monitoring transfer times for residents diagnosed with COVID-19, and tracking that residents who were transferred for COVID-19 care returned to their original neighborhood (see appendix C). The action plan was completed on February 28, 2021.
The Acting ADPCS conveyed that following the OIG’s virtual site visit in December 2020, concerns previously identified by administrative nurses who provided direct resident care during the CLC outbreak were provided to a Patient Clinical Support Workgroup and translated into a
VA OIG 21-00553-285 | Page 29 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
facility post-COVID-19 CLC outbreak action plan with recommendations and actions to address the concerns. A review of documentation provided showed the concerns were organized into the categories of communication, resources and assets, safety and security, staff responsibilities, utilities management, and patient clinical support. Each category had a team assigned to address the action items. An email to the OIG confirmed the teams were comprised of members from quality management, service chiefs, as well as executive and CLC leaders, and that direct care staff from the CLC were not included as members. The action items were discussed and monitored during updates provided to members of the command center. Representatives from the CLC were invited guests at a February 2021 command center meeting where CLC testing was discussed and reports from the workgroups were presented. Facility leaders’ post-COVID-19 outbreak action plan had several recommendations centered around communication; however, in only having the action plan presented to the command center team, an opportunity was missed to educate staff on actions being taken to prepare for a future outbreak. While the action plan was a step in the right direction, the plan was reliant on the observations from a limited number of staff and did not include direct care staff from the CLC.
In addition to the CLC COVID-19 upsurge action plan and facility post-COVID-19 outbreak action plan, the OIG learned the facility updated COVID-19 processes since the CLC outbreak focusing on screening, testing, isolation, and vaccination. Employee Health created a staff decision tree that provides situation-based guidance related to staff reports of exposure or symptoms. In December 2020, a facility document was created that states each CLC direct care staff member will be tested twice a week for COVID-19. The Geriatrics and Rehabilitation Service Chief issued a CLC SOP on February 18, 2021, outlining that residents would be tested twice a month. Additionally, the SOP outlined that when a resident tested positive, the resident would be isolated, and the service line chief would make a decision on the transfer of the resident based upon the resident’s condition. The SOP is silent on the time frame in which the isolation or decision to transfer will be made.
The facility made significant progress toward mitigation of the spread of COVID-19 with all CLC residents fully vaccinated as of March 9, 2021. The facility did not have the same success with facility staff vaccination rates. As of March 9, 2021, for the 1500 facility staff, the overall vaccination rate was 57 percent.
The OIG conducted a follow up interview with the Facility Director concerning post-CLC outbreak challenges and actions taken. The Director acknowledged challenges. The Director expressed concerns with both the facility culture and unit level accountability for actions. The Director and the executive team have taken action to work with consultants to assist with changing the organizational culture, and improving psychological safety and communication. The Director also shared that facility leaders were working with VHA to launch a program on leadership to be presented to all managers in the facility.
VA OIG 21-00553-285 | Page 30 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
As evidenced by the creation of action plans, facility and CLC leaders recognized the opportunity to make improvements following the CLC outbreak. The OIG noted the action planning process lacked involvement of ancillary and frontline staff to assist in identifying necessary corrective actions and opportunities for improvement.
Conclusion
The OIG substantiated that facility leaders and staff failed to observe general infection control practices specifically related to respiratory PPE. The OIG found CLC residents did not consistently wear face coverings prior to the CLC outbreak and some CLC staff did not comply with infection control measures related to face masks both prior to and after the CLC outbreak.
At the time of the CLC outbreak, the facility’s Environmental and Safety Section did not identify CLC providers and nursing staff as requiring respiratory protection. The OIG found that prior to the CLC outbreak some CLC providers, but none of the CLC nursing staff on the impacted units, were fit tested or trained. Additionally, a small percentage of nursing staff on Unity and Victory
were fit tested and none had PAPR training prior to the outbreak. The OIG concluded that nursing leaders and the Chief of Geriatrics and Rehabilitation Service failed to reassess the need for fit testing of CLC nursing staff. This failure resulted in CLC nursing staff providing direct patient care to residents with suspected and confirmed diagnoses of COVID-19 without the preferred respiratory protection.
The OIG substantiated that CLC and facility leaders failed to minimize the risk of CLC residents’ and staff exposure to COVID-19. The OIG found facility leaders did not follow CDC guidelines when responding to a CLC staff member’s reported cough and COVID-19 community close contact exposure and did not remove the employee from direct patient care. The facility did not have a comprehensive plan that specified operational details such as roles, actions, and targeted time frames for the transfer and isolation of CLC residents suspected of having or diagnosed with COVID-19. At the start of the CLC outbreak, two CLC residents were diagnosed with COVID-19, one of whom lived in a shared room. The OIG found that for the resident who shared a room, the resident’s roommate, who was not diagnosed with COVID-19 but was exposed, was not isolated. The transfer of the two CLC residents diagnosed with COVID-19 occurred 20 hours after the physician first became aware of both residents’ positive COVID-19 tests. The OIG confirmed the shared room of the non-infected resident was cleaned after the transfer of the roommate diagnosed with COVID-19; however, due to the non-functional bed management system and the absence of a substitute record keeping system, the OIG was unable to determine what time the room was cleaned.
The OIG determined that facility and CLC leaders did not implement the additional infection control measures recommended by the CDC when administering aerosol-generating procedures. CLC leaders also permitted group therapy sessions to continue throughout the pandemic thereby increasing residents and staff risk of exposure to COVID-19. However, CLC leaders minimized
VA OIG 21-00553-285 | Page 31 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
the risk of cross-contamination by ensuring staff did not work on both the COVID-19 and non COVID-19 designated units during the same shift.
The OIG found the facility lacked a plan for post-baseline testing of residents and staff. Additionally, the OIG substantiated that ongoing testing for residents and staff was inconsistent following the CLC outbreak. The OIG did not substantiate that facility staff failed to notify residents or their POCs, and staff of COVID-19 test results.
The OIG team identified a failure by facility leaders to proactively develop and implement plans to prepare for, and respond to, a potential COVID-19 outbreak at the CLC following VHA’s identification of the CLC as a high-risk environment. The OIG found the facility’s initial action plan, prepared prior to the official recognition of the pandemic and inception of the command center, lacked planning specific to CLC preparedness for mitigating or responding to COVID-19. Rather, facility leaders focused on planning for an influx of VHA patients from other geographic regions or non-VHA patients from the community who may have needed to be quarantined at the facility due to a lack of beds elsewhere. Facility leaders did not initiate CLC-specific planning until the CLC outbreak occurred, seven months into the pandemic. This failure to proactively develop and implement plans was a missed opportunity to ensure that facility and CLC staff were in a state of ongoing readiness should a CLC resident or staff member become diagnosed with COVID-19.
As evidenced by the creation of action plans, facility and CLC leaders recognized the opportunity to make improvements following the CLC outbreak. The OIG determined that the action planning process lacked involvement of ancillary and frontline staff to assist in identifying necessary corrective actions and opportunities for improvement.
The facility made significant progress toward mitigation of the spread of COVID-19 with all CLC residents fully vaccinated as of March 9, 2021. The facility did not have the same success with facility staff vaccination rates. As of March 9, 2021, for the 1500 facility staff, the overall vaccination rate was 57 percent.
VA OIG 21-00553-285 | Page 32 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
Recommendations 1–15
1. The VA Great Lakes Health Care System Director evaluates whether administrative action is warranted for individuals regarding failures to mitigate risk and manage a COVID-19 outbreak at the VA Illiana Health Care System, and takes action, as appropriate.
2. The VA Illiana Health Care System Director ensures the plan to monitor and track face mask wearing by staff at the community living center adheres to current Centers for Disease Control and Prevention guidance, is ongoing, results are monitored, and action plans are implemented as warranted.
3. The VA Illiana Health Care System Director confirms that all community living center staff identified as requiring respiratory protection are fit tested, trained, and have ready access to respiratory devices.
4. The VA Illiana Health Care System Director ensures a plan is in place that adheres to current Centers for Disease Control and Prevention guidance regarding staff with known community exposure to COVID-19, and monitors for compliance.
5. The VA Illiana Health Care System Director confirms that a comprehensive plan is in place that adheres to current Centers for Disease Control and Prevention guidance regarding community living center residents with known exposure to individuals diagnosed with COVID 19, and monitors compliance.
6. The VA Illiana Health Care System Director ensures operability and use of the bed management system for tracking completion of room cleaning.
7. The VA Illiana Health Care System Director oversees the completion and implementation of a policy for administering aerosol-generating procedures during the COVID-19 pandemic that adheres to Centers for Disease Control and Prevention guidance, and monitors compliance.
8. The VA Illiana Health Care System Director evaluates the organizational approach for notifying managers of updated Veterans Health Administration policies and guidance for monitoring actions taken to ensure compliance with new requirements.
9. The VA Illiana Health Care System Director reinforces facility staff understanding of Veterans Health Administration guidance related to community living center practices, including group activities, disseminated during emergent events such as a pandemic and maintains oversight of community living center leaders’ implementation of such guidance.
10. The VA Illiana Health Care System Director directs community living center leaders to complete a post-baseline plan for the COVID-19 disease that includes the required elements of screening, monitoring, and testing.
11. The VA Illiana Health Care System Director evaluates the community living center standard operating procedure titled “COVID-19 Bi-Monthly Resident Surveillance Testing”
VA OIG 21-00553-285 | Page 33 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
to ensure that it provides guidance with specific actions for staff to take when a resident tests positive for COVID-19.
12. The VA Illiana Health Care System Director verifies that COVID-19 testing for community living center residents and staff occurs as required for both routine surveillance and in response to confirmed cases of COVID-19.
13. The VA Illiana Health Care System Director confirms that the community living center COVID-19 standard operating procedure clearly communicates the process, including roles and responsibilities, for notification of a resident’s change in condition or room assignment and communicates the plan to all community living staff.
14. The VA Illiana Health Care System Director executes a process to ensure that the facility identifies potential high-risk scenarios, such as an outbreak of COVID-19 at the community living center, and when identified, creates a plan to mitigate and manage risk.
15. The VA Illiana Health Care System Director directs those conducting the facility’s after-action review of the community living center outbreak to include input from frontline community living center staff and takes action as necessary.
VA OIG 21-00553-285 | Page 34 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
Appendix A: Facility Campus Map
Green 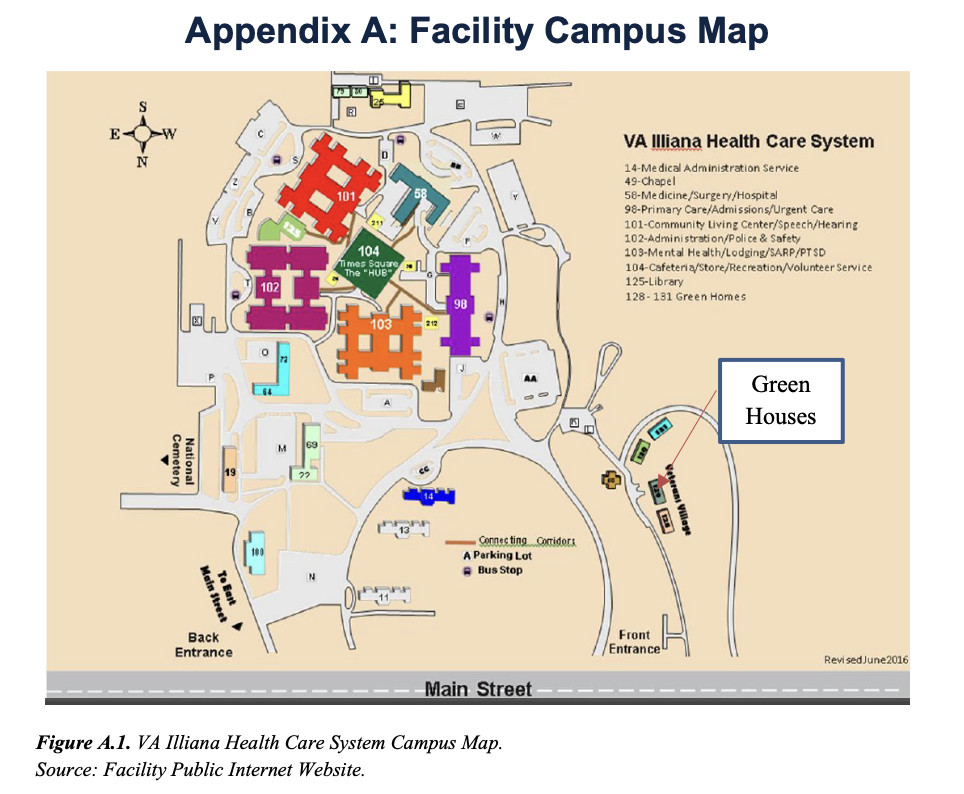
Houses
Figure A.1. VA Illiana Health Care System Campus Map.
Source: Facility Public Internet Website.
Table A.1. Neighborhood Call Names and Physical Locations
| CLC Neighborhood Call Name | Physical Location |
| 101-1 (unnamed) | Building 101 (CLC unit not in use prior to the outbreak) |
| 101-2 (unnamed) | Building 101 (CLC unit not in use prior to the outbreak) |
| Abe Lincoln | Building 101, unit 3 (101-3) |
| Stars and Stripes | Building 101, unit 4 (101-4) |
| Unity | Building 101, unit 7 (101-7) |
| Victory | Building 101, unit 8 (101-8) |
| Valor House | Building 131, Green House |
| Freedom House | Building 128, Green House |
| Honor House | Building 130, Green House |
| Liberty House | Building 129, Green House |
Source: OIG interviews with staff and facility provided internal documents.
VA OIG 21-00553-285 | Page 35 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
Appendix B: Facility Inpatient Surge Plan
October 22, 2020
Illiana Comprehensive Inpatient COVID-19 Surge Plan
Plan A: 58-2 2 Acute Care beds
1. Use two negative pressure beds 244, 246
2. Admit COVID positive/all levels of care (Acute, CLC, Mental Health)
3. Two additional rooms maybe used utilizing hepa-filters inside room
Plan B: Valor House CLC for non-Acute Veterans and continue with 58-2 for Acute Veterans (Acute, Mental Health)
1. Activate when COVID census reaches 3
2. Use available rooms 105, 109, 110, 114, 115, 117, 118, 122,123, 124
3. Provides a total of 10 COVID beds Valor and 2 Negative Pressure COVID beds on 58-2 4. These 10 rooms in Valor are private rooms and private bathrooms would NOT be negative pressure.
5. Notify VISN assessment of current conditions and staffing issues if applicable Plan C: Activate 101-2 Beds non-Acute 24 COVID beds. Continue to have available 2 Acute beds 58-2
1. Activate when COVID census reaches 10
2. Use 101-2 for COVID non-acute 102b (beds 2,3,4), 103b (beds 2,3,4), 104b (beds 1,2,3), 109b (2,3,4), 110b (beds 2,3,4), 111b (beds 2,3,4), 118b, 119b,120b,121b,122b,123b 3. Provides a total of 24 non-Acute COVID beds utilizing hepa-filters in hallways with two additional 58-2 Acute COVID negative pressure rooms
4. Assess staffing needs. Activate/continue Surge Staffing/Staff Mobilization plan if appropriate. Request VISN support if staffing is low.
Plan D: Consider decreasing services.
1. Curtail Services at recommendation of QUAD
2. Discuss mobilization of Veterans
VA OIG 21-00553-285 | Page 36 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
Appendix C: CLC Upsurge Action Plan Table C.1. October 22, 2020 CLC Upsurge Action Plan
State the /Issue Resolution/Actions to Be Taken
(include action words
and target dates)
Responsible Party/Parties
How Will this be Monitored
Status/Completion Date
Patients within the CLC are
testing positive for COVID19, presumably from staff exposure.
Educate staff:
1.Face to face
education by
Neighborhood Nurse Manager to be
provided regarding appropriate mask wearing.
1. Nurse Manager 1. Shift Nurse Manager will request staff
signature after face-to
face education, To
capture more
employees this will be
done two times in one
week per
neighborhood.
1.Goal date 11/6/2020 100% 11/24/2020
2.Provide hand out of an article for Correct Donning & Doffing of PPE:
https://www.cdc.gov/c oronavirus/2019-
ncov/downloads/A_F S_HCP_COVID19_P PE.pdf
3.Clinical staff will complete TMS,
“COVID19 Clinical Staff” TMS 41327
4.Complete TMS “COVID-19 PPE
Donning and Doffing Simulation” VA
41571.
Observation:
5.Neighborhood
Provider will audit five staff per week for appropriate mask wearing.
2. Neighborhood MAS & Nurse Manager
3. Nurse Managers & Neighborhood MAS
4. Nurse Managers & Neighborhood MAS
5. Neighborhood
Providers
2. Educational Read & Sign Notebook
3. TMS Completion Report
4. TMS Completion Report
5. Percentage of
compliant staff will be reported to Geriatrics and Rehabilitation Service Secretary weekly until three consecutive weeks at 100% or better are achieved.
2.Goal date 11/12/2020 100% 11/24/2020
3. Goal date 0/30/2020 11/30/2020: 120/149 81% 12/31/20: 140/145 97% 1/22/21: 145/145=100%
4.Goal date 11/12/2020 11/30/2020: 28/44 64% 12/31/20: 41/42 98% 1/21/21: 42/42=100%
5.100% compliance with correct mask wearing for 3 consecutive weeks.
October through December 100% COMPLETED
VA OIG 21-00553-285 | Page 37 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
State the /Issue Resolution/Actions to Be Taken
(include action words
and target dates)
Mitigation
Measures:
6.When testing
positive, Veterans will
be moved to the
appropriate
Neighborhood, such
as Valor, within the
shift; including after
hours, holidays and
weekends. This is to
reduce further staff
and Vet exposure.
7.Vets will return to
their usual
Neighborhood when
they are at minimum
meeting CDC criteria,
when clinically and
institutionally
appropriate.
Responsible
Party/Parties
6.Neighborhood Provider or Hospitalist On Call
7.COVID Neighborhood Provider
How Will this be
Monitored
6. QM RN CLC Liaison will audit transfer time of COVID19 positive Veterans.
7. COVID
Neighborhood Provider will observe symptoms and testing when
indicated
Status/Completion Date
6.100% for 3 consecutive months, November 2020 4/4 100%, December 2020 1/1 100%, January 2021 2/2 100% COMPLETED
7.100% for 3 consecutive months, November 2020: 18/20 90%, December 2020: 1/1 100%, January 2021: 0/0, February 2021: 3/3 100%
COMPLETED
Source: Facility CLC completed action plan on October 22, 2020.
VA OIG 21-00553-285 | Page 38 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
Appendix D: VISN Director Memorandum
Department of Veterans Affairs Memorandum
Date: September 9, 2021
From: Director, VA Great Lakes Health Care System (10N12)
Subj: Healthcare Inspection—Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at VA Illiana Health Care System in Danville, Illinois
To: Director, Office of Healthcare Inspections, (54HL05)
Director, GAO/OIG Accountability Liaison Office (VHA 10BGOAL Action)
1. Thank you for the opportunity to view the draft report of the VA Illiana Health Care System inspection. I would like to thank the OIG Inspection team for a thorough review.
2. I concur with recommendations 1-14 and support the facility response for 15.
3. Should you have additional questions, please contact the Quality Management Officer (QMO), VISN 12: VA Great Lakes Health Care System.
(Original signed by: Victoria P. Brahm, MSN, RN, VHA-CM)
VA OIG 21-00553-285 | Page 39 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
VISN Director Response
Recommendation 1
The VA Great Lakes Health Care System Director evaluates whether administrative action is warranted for individuals regarding failures to mitigate risk and manage a COVID-19 outbreak at the VA Illiana Health Care System, and takes action, as appropriate.
Concur.
Target date for completion: March 31, 2022
Director Comments
The VA Great Lakes Health Care System Director has initiated a Fact Finding to determine if administrative action is warranted for individuals who failed to mitigate risk and manage the COVID-19 outbreak at VA Illiana Health Care System. The Fact Finding team is charged to also make recommendations based on the findings.
VA OIG 21-00553-285 | Page 40 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
Appendix E: Facility Director Memorandum
Department of Veterans Affairs Memorandum
Date: September 9, 2021
From: Acting Director, VA Illiana Health Care System (550/00)
Subj: Healthcare Inspection—Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at VA Illiana Health Care System in Danville, Illinois
To: Network Director, Great Lakes VA Health Care Network (10N12)
1. Thank you for the opportunity to review the Office of the Inspector General (OIG) draft report “Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at VA Illiana Health Care System in Danville, Illinois.”
2. We extend our condolences to the family and friends of our patients and are deeply saddened by their loss. The cases in our Community Living Center impacted our entire staff and reinforced our commitment to learning and improving from the experience. As health care professionals, we find it difficult to accept the loss, especially as our staff were heavily invested in providing quality care and maintaining patient and staff safety throughout this pandemic.
3. We thank the OIG team for their recommendations which identified areas for improvement. We have been actively working to improve care for our Community Living Center Veterans and staff during the COVID-19 pandemic since the completion of our internal reviews. We concur with recommendations 2-14 and concur in principle with recommendation 15. The leadership team at VA Illiana Health Care System is committed to implementing corrective actions and will diligently pursue all measures to ensure safe, high-quality care for the Veterans that we serve.
(Original signed by:)
Staci M. Williams, Pharm D, RPh
Acting Medical Center Director
VA OIG 21-00553-285 | Page 41 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
Facility Director Response
Recommendation 2
The VA Illiana Health Care System Director ensures the plan to monitor and track face mask wearing by staff at the community living center adheres to current Centers for Disease Control guidance, is ongoing, results are monitored, and action plans are implemented as warranted.
Concur.
Target date for completion: March 31, 2022
Director Comments
The Acting VA Illiana Health Care System Director will ensure that the plan to monitor and track face mask wearing by staff in the Community Living Center adheres to current Centers for Disease Control guidance, is ongoing, results are monitored, and action plans are implemented as warranted. Statistics from personal protective equipment (PPE) rounding/tracers will be tracked and reported to Oversight Response Committee, of which the Acting Medical Center Director is the Chair, on a monthly basis until 6 months of 90% compliance are documented. Compliance is measured by number of staff compliant with PPE (numerator) as compared to total number of staff observed (denominator).
Recommendation 3
The VA Illiana Health Care System Director confirms that all community living center staff identified as requiring respiratory protection are fit tested, trained, and have ready access to respiratory devices.
Concur.
Target date for completion: October 31, 2021
Director Comments
The Acting VA Illiana Health Care System Director will confirm that all Community Living Center staff identified as requiring respiratory protection are fit tested, trained, and have ready access to respiratory devices. On February 23, 2021, the facility formally expanded the respiratory protection program to Community Living Center staff and fit testing and training was initiated for the staff members. Confirmation of compliance will be reported through the Oversight Response Committee, of which the Acting Medical Center Director is the Chair, at the October 2021 meeting. Compliance will be demonstrated by providing a list of names of the staff in two (2) representative CLC neighborhoods who require testing per policy and their testing and
VA OIG 21-00553-285 | Page 42 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
training dates. Since staff may change across the year, this item shall be considered closed once 100% of applicable staff onboard during the month of review have been tested and trained.
Recommendation 4
The VA Illiana Health Care System Director ensures a plan is in place that adheres to current Centers for Disease Control guidance regarding staff with known community exposure to COVID-19, and monitors for compliance.
Concur.
Target date for completion: October 31, 2021
Director Comments
The Acting VA Illiana Health Care System Director validated that a plan with ongoing monitoring is currently in place that adheres to current Centers for Disease Control guidance regarding staff with known community exposure to COVID-19. The facility developed a “COVID-19 Employee Decision Tree” that addresses staff with known exposure to COVID-19. Confirmation of compliance will be reported through Oversight Response Committee, of which the Acting Medical Center Director is the Chair, at the October 2021 meeting. Compliance will be measured by incorporating and communicating updates over six months of monitoring. Months with no cases will be counted as compliant with the intent of closing the finding within six months.
Recommendation 5
The VA Illiana Health Care System Director confirms that a comprehensive plan is in place that adheres to current Centers for Disease Control guidance regarding community living center residents with known exposure to individuals diagnosed with COVID-19, and monitors compliance.
Concur.
Target date for completion: September 30, 2021
Director Comments
On March 3, 2021, the facility revised its Standard Operating Procedure (SOP 11-83) “Outbreak Identification Control Management and Investigation” to ensure adherence to Centers for Disease Control guidance regarding Community Living Center residents with known exposure to individuals diagnosed with COVID-19. Confirmation of compliance will be reported through Oversight Response Committee, of which the Acting Medical Center Director is the chair, at the September 2021 meeting. Compliance will be measured by incorporating and communicating
VA OIG 21-00553-285 | Page 43 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
updates over six months of monitoring. Months with no modifications will be counted as compliant with the intent of closing the finding within six months.
Recommendation 6
The VA Illiana Health Care System Director ensures operability and use of the bed management system for tracking completion of room cleaning.
Concur.
Target date for completion: October 31, 2021
Director Comments
The Acting VA Illiana Health Care System Director ensures operability and use of the bed management system for tracking completion of room cleaning. The facility created a workgroup tasked with ensuring functionality and use of the bed management system. Confirmation of compliance will be reported through Oversight Response Committee, of which the Acting Medical Center Director is the chair, at the October 2021 meeting.
Recommendation 7
The VA Illiana Health Care System Director oversees the completion and implementation of a policy for administering aerosol-generating procedures during the COVID-19 pandemic that adheres to Centers for Disease Control guidance, and monitors compliance.
Concur.
Target date for completion: December 31, 2021
Director Comments
The facility has adopted VHA Guidance on Aerosol Generating Procedures During COVID-19 Outbreak. Confirmation of compliance will be reported monthly through Oversight Response Committee, of which the Acting Medical Center Director is the chair, until 6 months of 90% compliance is achieved. Compliance is measured by number of Veterans not receiving Aerosol Generating Procedures in the CLC (numerator) as compared to total number of Veteran charts traced per month in the CLC (denominator).
VA OIG 21-00553-285 | Page 44 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
Recommendation 8
The VA Illiana Health Care System Director evaluates the organizational approach for notifying managers of updated Veterans Health Administration policies and guidance for monitoring actions taken to ensure compliance with new requirements.
Concur.
Target date for completion: September 30, 2021
Director Comments
The Acting VA Illiana Health Care System Director has evaluated the organizational approach for notifying managers of updated Veterans Health Administration policies and guidance for monitoring actions taken to ensure compliance with new requirements. Opportunities for improvement were noted and new processes were implemented. Confirmation of completion will be reported through Oversight Response Committee, of which the Acting Medical Center Director is the chair, at the September 2021 meeting.
Recommendation 9
The VA Illiana Health Care System Director reinforces facility staff understanding of Veterans Health Administration guidance related to community living center practices, including group activities, disseminated during emergent events such as a pandemic and maintains oversight of community living center leaders’ implementation of such guidance.
Concur.
Target date for completion: October 31, 2021
Director Comments
The Acting VA Illiana Health Care System Director will utilize the same communication process referenced in the response to Recommendation 8 to reinforce facility staff understanding of VHA guidance related to Community Living Center practices, including group activities, disseminated during emergent events such as a pandemic and maintain oversight of Community Living Center
leaders’ implementation of such guidance. Ten random end user audits will be completed to ensure the information is being conveyed and that guidance is being followed. Confirmation of completion will be reported through Oversight Response Committee, of which the Acting Medical Center Director is the chair, at the October 2021 meeting.
VA OIG 21-00553-285 | Page 45 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
Recommendation 10
The VA Illiana Health Care System Director directs community living center leaders to complete a post-baseline plan for the COVID-19 disease that includes the required elements of screening, monitoring, and testing.
Concur.
Target date for completion: September 30, 2021
Director Comments
The Acting VA Illiana Health Care System Director will direct community living center leaders to complete a post-baseline plan for the COVID-19 disease that includes the required elements of screening, monitoring, and testing. The facility standard operating procedure “COVID-19 Testing Residents/Staff” was reviewed and opportunities for improvement were identified. Confirmation of compliance will be reported through Oversight Response Committee, of which the Acting Medical Center Director is the chair, at the September 2021 meeting.
Recommendation 11
The VA Illiana Health Care System Director evaluates the community living center standard operating procedure titled “COVID-19 Bi-Monthly Resident Surveillance Testing” to ensure that it provides guidance with specific actions for staff to take when a resident tests positive for COVID-19.
Concur.
Target date for completion: September 30, 2021
Director Comments
The Acting VA Illiana Health Care System Director will evaluate the Community Living Center standard operating procedure titled “COVID-19 Bi-Monthly Resident Surveillance Testing” to ensure that it provides guidance with specific actions for staff to take when a resident tests positive for COVID-19. Confirmation of compliance will be reported through Oversight Response Committee, of which the Acting Medical Center Director is the chair, at the September 2021 meeting.
VA OIG 21-00553-285 | Page 46 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
Recommendation 12
The VA Illiana Health Care System Director verifies that COVID-19 testing for community living center residents and staff occurs as required for both routine surveillance and in response to confirmed cases of COVID-19.
Concur.
Target date for completion: December 31, 2021
Director Comments
The Acting VA Illiana Health Care System Director will verify that COVID-19 testing for community living center residents and staff occurs as required for both routine surveillance and in response to confirmed cases of COVID-19. The facility has an established tracking system to ensure testing occurs as required. Confirmation of compliance will be reported monthly through Oversight Response Committee, of which the Acting Medical Center Director is the chair, until 6 months of 90% compliance is achieved. Compliance is measured by number of community living center residents and staff receiving testing in compliance with policy (numerator) as compared to total number of residents and staff (denominator).
Recommendation 13
The VA Illiana Health Care System Director confirms that the community living center COVID 19 standard operating procedure clearly communicates the process, including roles and responsibilities, for notification of a resident’s change in condition or room assignment and communicates the plan to all community living staff.
Concur.
Target date for completion: October 31, 2021
Director Comments
Community Living Center standard operating procedure #11-83, Outbreak Identification Control Management and Investigation, was reviewed and opportunities for improvement identified. Confirmation of compliance will be reported through Oversight Response Committee, of which the Acting Medical Center Director is the chair, at the September 2021 meeting.
VA OIG 21-00553-285 | Page 47 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
Recommendation 14
The VA Illiana Health Care System Director executes a process to ensure that the facility identifies potential high-risk scenarios, such as an outbreak of COVID-19 at the Community Living Center, and when identified, creates a plan to mitigate and manage risk.
Concur.
Target date for completion: October 31, 2021
Director Comments
The Acting VA Illiana Health Care System Director will execute a process to ensure that the facility identifies potential high-risk scenarios, such as an outbreak of COVID-19 at the Community Living Center, and when identified, creates a plan to mitigate and manage risk. The Emergency Operations Plan, SOP 001ESS-05, will be reviewed and modified to include a process to identify potential risks and mitigation/management strategies. The current facility process upon identification of an issue is to convene a team of subject matter experts to conduct a risk assessment based on the type of event, intervene to mitigate the risks, and monitor compliance will be added to the Emergency Operations Plan. Confirmation of completion will be reported through Oversight Response Committee, of which the Acting Medical Center Director is the chair, at the October 2021 meeting.
Recommendation 15
The VA Illiana Health Care System Director directs those conducting the facility’s after action review of the Community Living Center outbreak to include input from frontline community living center staff and takes action as necessary.
Concur in principle.
Target date for completion: September 30, 2021
Director Comments
The facility had developed six core workgroups following the October/November Community Living Center outbreak. Each workgroup consulted and/or included frontline staff members when developing facility action plans. In addition, listening sessions were held on February 1, 2021 following the outbreak to obtain feedback from frontline staff. Actions identified by the workgroups or through listening sessions have been completed. Confirmation of compliance will be reported through Oversight Response Committee, of which the Acting Medical Center Director is the chair, at the September 2021 meeting.
VA OIG 21-00553-285 | Page 48 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
Glossary
aerosol-generating procedure. Procedures that are believed to spray mist and droplets as a source of respiratory pathogen and can include “positive pressure ventilation (BiPaP and CPAP), endotracheal intubation, airway suction, high frequency oscillatory ventilation, tracheostomy, chest physiotherapy, nebulizer treatment, sputum induction, and bronchoscopy.”71
baseline testing. Initial viral testing of a resident or individual “who is not known to have previously been diagnosed with COVID-19.”72
close contact. “Someone who has been within 6 feet of an infected person…for a cumulative total of 15 minutes or more over a 24-hour period…. An infected person can spread SARS-CoV 2 [COVID-19] starting from 2 days before they have any symptoms (or, for asymptomatic patients, 2 days before the positive specimen collection date) until they meet criteria for discontinuing home isolation.”73
contact tracing. The practice of identifying, notifying, and monitoring individuals who may have had close contact with a person having a confirmed or probable case of an infectious disease as a means of controlling the spread of infection.74
continuous positive airway pressure. “A treatment that uses mild air pressure to keep your breathing airways open.” It involves using a “machine that includes a mask or other device that fits over your nose or your nose and mouth, straps to position the mask, a tube that connects the mask to the machine’s motor, and a motor that blows air into the tube.”75
COVID-19. “Coronavirus disease 2019 (COVID-19) is caused by a new coronavirus first identified in Wuhan, China, in December 2019. Because it is a new virus, scientists are learning more each day. Although most people who have COVID-19 have mild symptoms, COVID-19
71 Tran, Khai et al., “Aerosol Generating Procedures and Risk of Transmission of Acute Respiratory Infections to Healthcare Workers: A Systematic Review.” PLoS ONE vol. 7,4 (2012): e35797. doi:
10.1371/journal.pone.0035797
72“Testing Guidelines for Nursing Homes: Interim SARS-CoV-2 Testing Guidelines for Nursing Home Residents and Healthcare Personnel,” CDC, accessed February 24, 2021, https://www.cdc.gov/coronavirus/2019- ncov/hcp/nursing-homes-testing.html.
73“COVID-19, Appendices,” CDC, accessed on April 29, 2021, https://www.cdc.gov/coronavirus/2019- ncov/php/contact-tracing/contact-tracing-plan/appendix.html.
74 Merriam Webster ”Definition of contact tracing” accessed March 25, 2021, https://www.merriam webster.com/dictionary/contacttracing
75 “CPAP,” National Heart, Lung, and Blood Institute, accessed February 25, 2021,
https://www.nhlbi.nih.gov/health-topics/cpap.
VA OIG 21-00553-285 | Page 49 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
can also cause severe illness and even death. Some groups, including older adults and people who have certain underlying medical conditions, are at increased risk of severe illness.”76
fit testing. “The use of a protocol to qualitatively or quantitatively evaluate the fit of a respirator on an individual.”77
geri-psychiatric. “Geriatric psychiatry emphasizes the biological and psychological aspects of normal aging, the psychiatric effect of acute and chronic physical illness, and the biological and psychosocial aspects of the pathology of primary psychiatric disturbances of older age.”78
n95. A type of National Institute for Occupational Safety and Health (NIOSH)-approved filtering facepiece respirator (FFP). N95s are air purifying respirators that protects by filtering particles out of the air while the user is breathing. N95s filter at least 95% of airborne particles and is not resistant to oil.79
nebulizer. An atomizer equipped to produce an extremely fine spray for deep penetration of the lungs.80
negative pressure room. A form of hospital isolation room that “prevents airborne disease (such as tuberculosis or flu) from escaping the room.” “A machine pulls air into the room. Then it filters the air before moving it outside.”81
outbreak. “A recommended definition is a situation that is consistent with either of two sets of criteria: During (and because of) a case investigation and contact tracing, two or more contacts are identified as having active COVID-19, regardless of their assigned priority. OR Two or more patients with COVID-19 are discovered to be linked, and the linkage is established outside of a case investigation and contact tracing (e.g., two patients who received a diagnosis of COVID-19
76 CDC, About COVID-19, accessed April 29, 2021, https://www.cdc.gov/coronavirus/2019- ncov/cdcresponse/about-COVID-19.html.
77 National Institute for Occupational Safety and Health, National Personal Protective Technology Laboratory. Hospital Respiratory Protection Program Toolkit: Resources for Respirator Program Administrators, May 2015, Publication Number 2015-117.
78 “Geriatric Psychiatry,” American Psychiatric Association, accessed on February 24, 2021, https://www.psychiatry.org/psychiatrists/practice/professional
interests/geriatric#:~:text=Geriatric%20Psychiatry%20Geriatric%20psychiatry%20emphasizes%20the%20biologica l%20and,pathology%20of%20primary%20psychiatric%20disturbances%20of%20older%20age. 79 “NIOSH Guide to the Selection and Use of Particulate Respirators,” Centers for Disease Control and Prevention, accessed on February 23, 2021, https://www.cdc.gov/niosh/npptl/topics/respirators/disp_part/default.html. 80 Merriam Webster, “Definition of nebulizer,” accessed February 25, 2021, https://www.merriam webster.com/medical/nebulizer.
81 “Hospital Isolation Rooms,” Michigan Medicine, accessed on February 24, 2021,
https://www.uofmhealth.org/health-library/abo4381.
VA OIG 21-00553-285 | Page 50 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
are found to work in the same office, and only one or neither of the them was listed as a contact to the other).”82
palliative. “Specialized medical care for people living with a serious illness” that focuses on providing “relief from the symptoms and stress of the illness. The goal is to improve quality of life for both the patient and family.”83
pandemic. “An outbreak of a disease that occurs over a wide geographic area (such as multiple countries or continents) and typically affects a significant proportion of the population: a pandemic outbreak of a disease.”84
personal protective equipment. “Specialized clothing or equipment worn by an employee to protect the respiratory tract, mucous membranes, skin, and clothing from infectious agents or other hazards. Examples of PPE include gloves, respirators, goggles, facemasks, surgical masks, face shields, footwear, and gowns.”85
powered air purifying respirator. “An air purifying respirator that uses a blower to force air through filters or cartridges and into the breathing zone of the wearer. This creates a positive pressure inside the facepiece or hood, providing more protection than a non-powered or negative pressure half mask APR [air purifying respirator].”86
prevalence. “The degree to which something is prevalent especially: the percentage of a population that is affected with a particular disease at a given time.”87
respirator. “A mask or device worn over the mouth and nose to protect the respiratory system by filtering out dangerous substances (such as dusts, fumes, or bacteria) from inhaled air. NOTE: Particulate respirator masks are only able to filter out particles and are not effective against gases or vapors. A numerical rating (such as 95 or 99) is sometimes assigned to such a respirator to indicate the percentage of airborne particles filtered. A letter may also be assigned to indicate
82 “Managing Investigation During an Outbreak,” CDC, accessed February 24, 2021,
https://www.cdc.gov/coronavirus/2019-ncov/php/contact-tracing/contact-tracing-plan/outbreaks.html. 83 “About Palliative Care,” Center to Advance Palliative Care, accessed February 23, 2021, https://www.capc.org/about/palliative-care/.
84 Merriam Webster, “Definition of pandemic,” accessed July 20, 2021, https://www.merriam webster.com/dictionary/pandemic
85 National Institute for Occupational Safety and Health, National Personal Protective Technology Laboratory. Hospital Respiratory Protection Program Toolkit: Resources for Respirator Program Administrators, May 2015, Publication Number 2015-117.
86 National Institute for Occupational Safety and Health, National Personal Protective Technology Laboratory. Hospital Respiratory Protection Program Toolkit: Resources for Respirator Program Administrators, May 2015, Publication Number 2015-117.
87 Merriam Webster, “Definition of prevalence,” accessed August 9, 2021, https://www.merriam webster.com/dictionary/prevalence
VA OIG 21-00553-285 | Page 51 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
whether it is somewhat resistant (R), not resistant (NR), or strongly resistant (P) to the degrading effects of oil on proper respirator function.”88
source control. “Use of well-fitting cloth masks, facemasks, or respirators to cover a person’s mouth and nose to prevent spread of respiratory secretions when they are breathing, talking, sneezing, or coughing. Cloth masks, facemasks, and respirators should not be placed on children under age 2, anyone who cannot wear one safely, such as someone who has a disability or an underlying medical condition that precludes wearing a cloth mask, facemask, or respirator safely, or anyone who is unconscious, incapacitated, or otherwise unable to remove their cloth mask, facemask, or respirator without assistance. Face shields alone are not recommended for source control.”89
88 Merriam Webster, “Definition of respirator,” accessed July 20, 2021, https://www.merriam webster.com/dictionary/respirator.
89“Interim Infection Prevention and Control Recommendations for Healthcare Personnel During the Coronavirus Disease 2019 (COVID-19) Pandemic.”
VA OIG 21-00553-285 | Page 52 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
OIG Contact and Staff Acknowledgments
Contact For more information about this report, please contact the Office of Inspector General at (202) 461-4720.
Inspection Team Susan Tostenrude, MS, Director
Kevin Arnhold, FACHE
Leakie Bell-Wilson, MSN, RN
Tabitha Eden, MSN, RN
Nancy Short, LCSW
Thomas Wong, DO
Other Contributors Alicia Castillo-Flores, MBA, MPH
Christopher Dong, JD
Christopher Hoffman, LCSW, MBA
Carol Lukasewicz, BSN, RN
Sarah Mainzer, JD, BSN
Natalie Sadow, MBA
Robyn Stober, JD, MBA
Robert Wallace, MPH, ScD
VA OIG 21-00553-285 | Page 53 | September 28, 2021
Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at the VA Illiana Health Care System in Danville, IL
Report Distribution
VA Distribution
Office of the Secretary
Veterans Health Administration
Assistant Secretaries
General Counsel
Director, VA Great Lakes Health Care System (10N12)
Director, VA Iliana Health Care System (550)
Non-VA Distribution
House Committee on Veterans’ Affairs
House Appropriations Subcommittee on Military Construction, Veterans Affairs, and Related Agencies
House Committee on Oversight and Reform
Senate Committee on Veterans’ Affairs
Senate Appropriations Subcommittee on Military Construction, Veterans Affairs, and Related Agencies
Senate Committee on Homeland Security and Governmental Affairs
National Veterans Service Organizations
Government Accountability Office
Office of Management and Budget
U.S. Senate
Illinois: Tammy Duckworth, Richard J. Durbin
Indiana: Mike Braun, Todd Young
U.S. House of Representatives
Illinois: Mike Bost, Cheri Bustos, Rodney Davis, Bill Foster, Robin Kelly, Adam Kinzinger, Darin LaHood, Mary Miller
Indiana: Jim Baird, Larry Bucshon, Frank Mrvan
OIG reports are available at www.va.gov/oig
VA OIG 21-00553-285 | Page 54 | September 28, 2021





 Alerts Sign-up
Alerts Sign-up